While bone suppression techniques can help identify lung nodules on chest x-rays, computer-aided detection (CAD) software fails to improve radiologist performance, according to separate Web-exclusive studies published in the May edition of the American Journal of Roentgenology.
Thanks to its ability to reveal nodules obscured by bone on chest radiographs, bone suppression can significantly improve detection accuracy for subtle nodules, a University of Chicago study team concluded. Researchers from the Cleveland Clinic, however, determined that CAD did not improve the performance of chest or general radiologists, and it actually increased incorrect follow-up decisions by pulmonologists in their retrospective study.
Bone suppression
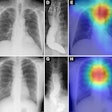
The superimposition of bones on chest radiographs can obscure lung nodules and is a major cause of missed lung cancers by radiologists. As a result, the Chicago team sought to compare the performance of radiologists using SoftView bone suppression imaging software, version 2.0 (Riverain Medical), in detecting subtle nodules (AJR, May 2011, Vol. 196:5, pp. W535-W541).
The researchers have been interested in image processing for chest radiography for many years, including techniques such as rib suppression, energy subtraction, and temporal subtraction, according to co-author Dr. Heber MacMahon. They collaborated with Riverain in developing the application and took the opportunity to test it in a simulated clinical environment, he said.
In the independent observer study, the researchers gathered digitized radiographs of 72 patients with a subtle nodule (47 malignant and 25 benign) and 79 patients without nodules from the Japanese Society of Radiological Technology nodule database. They then applied SoftView to the 151 radiographs to create bone suppression images.
Two image reading sets were created. The first included half of the patient population (subset A) showing only the standard image, and half (subset B) showing the standard image as well as bone suppression images. In the second reading set, bone suppression images were added to subset A, and subset B only included the standard images.
Three radiologists read the two image sets, with two weeks in between reading sessions. They also indicated their confidence levels regarding the presence of a lung nodule (on a scale from 0 to 10), and marked the most likely position for a nodule, if they thought it was present, for each image or image pair, according to the researchers. The study team then calculated receiver operator characteristics (ROC) curves to evaluate the radiologists' performance.
For the three observers, the mean area-under-the-curve (AUC) value of the ROC curves for detecting subtle lung nodules was 0.863 when using chest radiographs and bone suppression images, up from 0.840 with chest radiographs alone. The difference was statistically significant (p = 0.01).
In addition, the mean detection rate for subtle nodules climbed from 60% with chest radiographs alone to 64% with the addition of bone suppression images. On the downside, the mean number of false-positive findings increased from 18 with chest radiographs alone to 25 with the addition of bone suppression images.
"The key finding is that use of this bone suppression technique can significantly improve detection accuracy for lung nodules, which are commonly obscured by overlying ribs and clavicles," MacMahon told AuntMinnie.com. "However, we have also shown in a separate experiment that it can be useful for detection of focal pneumonia."
The bone suppression technique could be routinely used, just as dual-energy radiography has been routinely employed in their department for many years, MacMahon said.
"Because there is no additional radiation exposure or specialized equipment required, it can also be applied to bedside portable [chest x-rays]," he said.
CAD
In another Web-exclusive paper published in the May AJR, a research team led by Dr. Moulay Meziane, of the Cleveland Clinic, examined the effect of chest radiography CAD software on the follow-up recommendations of the three most common types of specialists who use chest radiographs in their clinical practice: chest radiologists, general radiologists, and pulmonologists.
In a large, retrospective study, the study team evaluated RapidScreen 1.1 chest radiography CAD software (Riverain), as well as a second-generation system, OnGuard 3.0 (Riverain), for analyzing single frontal radiographs of 200 patients judged to be at high risk for lung cancer. Of these, 100 had actionable nodules with a mean size of 16.9 mm, and 100 had no nodules (AJR, May 2011, Vol. 196:5, pp. W542-W549).
Eighteen readers, including six chest radiologists, six general radiologists, and six pulmonologists, participated in the study. Images were read first without CAD and then with both versions of CAD in a sequential reading format. RapidScreen 1.1 was used first in approximately half of the cases, while OnGuard 3.0 was used first for the rest.
On both the images without CAD and those with CAD, readers recorded the size and location of all possible solid nodules.
For pulmonologists, CAD led to a significant increase in follow-up recommendations for patients without actionable lesions (p = 0.001), while chest and general radiologists had much lower average rates and were not affected by CAD's false-positive marks, according to the researchers.
Percent of patients without actionable lesions recommended for follow-up
|
Among all readers, there was no significant difference in the frequency with which actionable nodules were recommended for follow-up, or between Rapid Screen 1.1 and OnGuard 3.0, which was not released commercially by Riverain..
Mean proportion of patients with actionable nodules recommended for follow-up
|
CAD did improve the detection rate of all readers for moderately subtle lesions, however (p = 0.013).
Overall, though, the Cleveland Clinic study results contradict findings from several large and small studies that found improvements in radiologists' performance with CAD. This may be due to the new study's design, which required readers with CAD to relocate and rescore all suspicious lesions, according to the authors.
"We did not locate or display for them their unaided findings while they interpreted the CAD marks," they wrote. "In other studies readers did not have to locate the suspicious lesions; they assigned one overall confidence score without CAD, and they were given this unaided confidence score and allowed to modify it once the CAD marks were displayed. It is possible that the latter approach makes it more likely for readers to increase their sensitivity with CAD. In contrast, our study design imposed on the readers to re-enter their findings to get credit for any lesions."
The way CAD is currently being used in radiology has potential to spur an increase in inappropriate recommendations by nonradiologist clinicians for additional testing, due to their tendency to believe some of the false-positive CAD marks, the researchers concluded.
"Furthermore, we found no significant improvement in lung cancer detection for general and chest radiologists using CAD," the authors wrote. "Until CAD reaches a high level of accuracy with a minimum number of false positives, it should not be universally adopted; instead, use should be based on the individual preferences of readers who see an objective improvement in their performance."