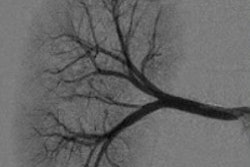
Spinal digital subtraction angiography (DSA) has acquired a reputation as a risky interventional procedure, but that notoriety is largely unfounded, according to a study by researchers from Johns Hopkins University that was published online September 14 in Neurology.
Spinal DSA is considered the gold standard for diseases of the spinal cord vasculature, such as strokes, hematomas, aneurysms, fistulas, and tumors. However, the technique is also considered to have a high rate of neurological complications, largely based on experiences prior to the 1970s, when spinal DSA was first introduced and the procedures used hyperosmotic, ionic contrast agents. Rates of stroke and kidney damage approached 3% at this time, according to the authors.
Nearly 40 years later, some clinicians are still reluctant to order spinal DSA exams, based largely on outdated information that has been rendered obsolete by advances in endovascular technology. Medical student James Chen and interventional neuroradiologist Dr. Philippe Gailloud sought to shed some light on the topic by studying 10 years of data on spinal DSA complications based on studies conducted at their hospital.
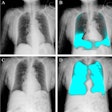
Chen and Gailloud reviewed a population of 302 consecutive spinal angiograms performed in 288 patients from 2000 to 2010 at Johns Hopkins. All studies were conducted with a dedicated neurological suite, and procedures were analyzed for the incidence of neurological, nonneurological, and local complications during or immediately after spinal DSA. Analyses were performed to find associations between complication rates and different variables such as patient age, gender, extent of disease, contrast dose, and fluoroscopy time.
The researchers found no evidence of intraprocedural or postprocedural neurological complications (0.0%, 95% confidence interval [CI]: 0.0%-1.2%). There was no evidence of iatrogenic vessel injury, and no transient or permanent neurological deficits related to thromboembolic events. There were also no cases of significant contrast allergy or nephrotoxicity (0.0%, 95% CI: 0.0%-1.2%).
Two patients developed nonneurological complications after spinal DSA (0.7%, 95% CI: 0.1%-2.4%). Local postprocedural complications included three groin hematomas (1.0%, 95% CI: 0.2%-2.9%).
The researchers found that 60 patients were diagnosed with a spinal vascular malformation. Of these, 41 (68%) were treated with surgery or endovascular embolization, and of the remaining 19, 12 (20%) were managed conservatively and seven (12%) were treated at outside institutions and lost to study follow-up.
The study results indicate that spinal DSA has a good safety profile, and it can be performed with minimal rates of neurological complications and limited contrast volumes and fluoroscopy exposure, the authors concluded. The procedure is able to confirm or exclude the presence of spinal vascular lesions with certainty and, thus, can continue to play a role in atypical or diagnostically challenging cases.