Women 65 years and older should be screened regularly for osteoporosis, according to a final recommendation from the U.S. Preventive Services Task Force (USPSTF) published in the June 26 issue of the Journal of the American Medical Association.
The task force also recommended that postmenopausal women younger than 65 who are at risk for the disease get regular screening. As for men, the USPSTF stated that there is insufficient evidence to support osteoporosis screening.
The update is consistent with the task force's previous guidance, released in 2011.
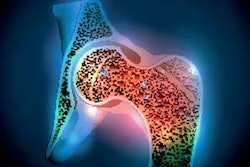
Osteoporosis is a key health issue, the USPSTF said: By 2020, more than 12 million people in the U.S. older than 50 are expected to have it. Fractures caused by the disease -- especially hip fractures -- can cause limited mobility, chronic pain and disability, loss of independence, and decreased quality of life (JAMA, June 26, 2018, Vol. 319:24, pp. 2521-2531).
"With the aging of the U.S. population, the potential preventable burden [of osteoporosis] is likely to increase in future years," the task force wrote. "[Because osteoporosis] is usually asymptomatic until a fracture occurs ... preventing osteoporotic fractures is the main goal of an osteoporosis screening strategy."
The most common test for osteoporosis screening is central dual-energy x-ray absorptiometry (DEXA), which measures bone mineral density (BMD) at the hip and lumbar spine, but other tests include peripheral DEXA and quantitative ultrasound. The USPSTF's main recommendation is geared toward adults without a history of low-trauma fractures and without conditions that may cause secondary osteoporosis (such as metabolic bone disease or untreated hyperthyroidism).
As for postmenopausal women younger than 65, the recommendation urges clinicians to consider factors associated with increased risk, such as parental history of hip fracture, smoking, excessive alcohol consumption, and low body weight. The guidance lists a number of tools that can be used to assess osteoporosis risk, including the Fracture Risk Assessment Tool (FRAX), the Simple Calculated Osteoporosis Risk Estimation (SCORE), the Osteoporosis Risk Assessment Instrument (ORAI), the Osteoporosis Index of Risk (OSIRIS), and the Osteoporosis Self-Assessment Tool (OST).
The task force left the selection of screening intervals to physician and patient discretion, noting that "some observational and modeling studies have suggested screening intervals based on age, baseline BMD, and calculated projected time to transition to osteoporosis. However, limited evidence from two ... studies found no benefit in predicting fractures from repeating bone measurement testing four to eight years after initial screening."
In an editorial in the same JAMA issue (pp. 2483-2485), Jane Cauley, PhD, of the University of Pittsburgh noted that mineral density screening is generally effective; however, because it does have some limitations, considering a patient's risk factors is important when determining how best and how often to screen for osteoporosis.
"Fracture prevention is the ultimate goal, and BMD screening is an effective, low-cost, noninvasive means of identifying men and women at high risk of fracture," she wrote. "Yet major deficiencies remain in BMD screening, even among women 65 years and older. Assessment of clinical risk factors is also important, because individuals with the combination of low BMD and an increasing number of risk factors have the highest incidence of hip fracture."