.png?auto=format%2Ccompress&q=70&w=400)
Just how well does radiography perform in detecting signs of COVID‑19? A range of recent studies indicates that while x-ray may not have the diagnostic power of CT, it still has a role to play in managing the pandemic.
Early reports from Wuhan, China, touted the role of CT in detecting changes in lung damage that can be telltale signs of infection with the SARS-CoV-2 virus. Radiography's value was called into question by a February 26 study from South Korea in which researchers found that x‑ray missed three-quarters of pulmonary nodules related to COVID-19 that were later found on CT.
But a review of some of the more recent literature finds that radiography actually can be useful for COVID-19 detection, once its limitations are known. X-ray is an inexpensive technology that's easy to operate, and its portability means it can be taken to the patient's bedside -- reducing the radiology department's exposure to infection.
And applying coming technologies like artificial intelligence (AI) could make radiography even more useful by enabling automated analysis of chest x-rays
What works, what doesn't
Like much of the news about COVID-19, new clinical studies on the use of x-ray in the pandemic have been coming fast and furious. Below are some of the more important studies.
Low sensitivity, high specificity. Radiography's sensitivity was only 25% when detecting lung opacities related to COVID-19, according to a March 30 study in Radiology: Cardiothoracic Imaging of 20 patients seen in South Korea by Dr. Hyewon Choi and colleagues. But the researchers found that radiography's specificity was 90% (March 30, 2020, Radiology: Cardiothoracic Imaging).
The researchers acknowledged that while CT might be the primary imaging modality for evaluating suspected COVID-19 cases, "it is operationally more complex to perform CT scans," especially when considering the scanner disinfection procedures that have to take place.
Choi et al undertook their study to try to measure radiography's effectiveness by comparing it with a quantitative value they called quantitative CT opacity mass, derived from software analysis of lung CT scans of the same patients who got x-ray studies. The values were compared with eight radiologists interpreting radiographs and identifying opacities they saw.
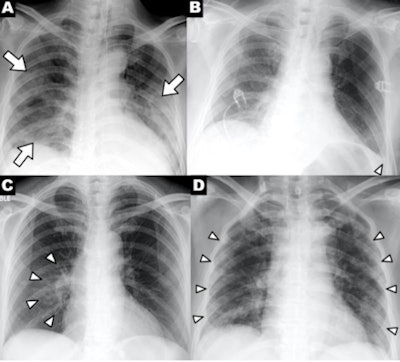 A series of chest x-ray findings of a patient with COVID-19 demonstrating clinical characteristics of disease: (A) patchy consolidations, (B) pleural effusion, (C) perihilar distribution, and (D) peripheral distribution. Images courtesy of RSNA.
A series of chest x-ray findings of a patient with COVID-19 demonstrating clinical characteristics of disease: (A) patchy consolidations, (B) pleural effusion, (C) perihilar distribution, and (D) peripheral distribution. Images courtesy of RSNA.The researchers said that clinicians should keep the study's findings in mind when interpreting chest x-rays of suspected COVID-19 patients, or when deciding which imaging modality to use.
"Clinicians and radiologists should keep in mind that a greater extent of disease can exist than that suggested by inspection of chest radiographs, and that chest radiographs may also have limitations for monitoring the disease extent," Choi et al concluded.
Lower sensitivity than DNA testing. Meanwhile, a March 27 study in Radiology found that radiography fared somewhat better, but it did not approach the sensitivity of DNA testing of COVID-19 patients. In this study by Dr. Frank Ho Yuen Wong and colleagues of Hong Kong, radiography turned in sensitivity of 69%, compared with 91% for DNA testing with reverse transcription polymerase chain reaction (RT-PCR) assay.
The researchers analyzed images from 64 patients who were seen at four Hong Kong hospitals from January-March 2020. They found that signs of COVID-19 on chest radiography were similar to those of CT: bilateral, peripheral consolidation and/or ground-glass opacities. Consolidation was the most common finding on x-ray in 47% of patients, while ground-glass opacities were found in 33%.
In another useful finding, Wong et al found that the severity of findings on chest x-ray of COVID-19 patients peaked at 10-12 days after the onset of symptoms. Interestingly, they found some evidence of COVID-19 in six patients who had negative RT-PCR tests, leading them to postulate that a positive chest x-ray could obviate the need for CT, reducing the workload on CT units.
Clinical features on radiography. What features on x-ray are indicative of COVID-19? Chest radiography can show patchy or diffuse asymmetric airspace opacities that are similar to pneumonia caused by other coronaviruses, according to a March 23 article by Dr. Jonathan Rodrigues, PhD, and colleagues in Clinical Radiology.
Meanwhile, researchers from the University of Washington in Seattle have provided a list of the top five findings on chest x-ray of COVID-19. The most common finding was bilateral reticular nodular opacities, found in 52% of cases, followed by ground-glass opacities in 48%. Some 72 hours after admission, these findings rose to 86% for reticular nodular opacities and 67% for ground-glass opacities, they wrote in a study published March 19 in JAMA.
Infection control and radiography. One of the advantages that radiography has for imaging COVID-19 patients is its portability. Mobile x-ray systems should always be used for patients suspected of having COVID-19, and a satellite radiology center with mobile x-ray equipment dedicated to COVID-19 imaging can even be set up closer to intensive care units, decreasing risk of virus transmission, according to Dr. Soheil Kooraki and colleagues in the April 2020 edition of the Journal of the American College of Radiology.
Meanwhile, the Clinical Radiology authors also weighed in on infection-control procedures, which also emphasize the use of portable x-ray systems. Systems should be in place to identify at-risk patients who might have COVID-19, radiology staff should be trained in disinfection procedures, and "clean" and "dirty" areas should be designated.
Portable x-ray also got a nod from an American College of Radiology (ACR) task force on COVID-19, which recommended the modality for use in ambulatory care facilities due to the ease with which surfaces can be cleaned, according to a March 11 recommendation. The ACR pronouncement further recommends that imaging facilities consider ventilation in rooms with fixed radiography systems or CT scanners -- rooms may need to be taken offline for about one hour between patients, depending on air circulation rates.
AI for x-ray of COVID-19. Radiography's move to digital imaging means that sophisticated image analysis tools once reserved for more advanced modalities can now be used for x-ray. And the most sophisticated of this is artificial intelligence (AI).
A team in Canada has developed an open-source AI algorithm called COVID-Net that's designed to detection the disease on chest radiographs. They say the convolutional neural network produced almost 100% sensitivity and 83% accuracy for COVID-19 on a small test dataset -- but more real-world testing is obviously needed. They published their work March 22 on arXiv.org.
As the novel coronavirus pandemic grinds on, clinicians on the front lines may increasingly turn to radiography
"As the COVID-19 pandemic threatens to overwhelm healthcare systems worldwide, [chest x-ray] may be considered as a tool for identifying COVID-19, but [it] is less sensitive than CT," Wong et al concluded in Radiology



















