Emergency departments may be able to triage high-risk COVID-19 patients on x-ray with the help of an artificial intelligence (AI) model, according to research published May 12 in npj Digital Medicine.
The researchers cited a pressing need during the COVID-19 pandemic for emergency department physicians and radiologists to quickly predict which COVID-19 patients are likely to have potentially fatal complications so that treatment resources can be matched to those at increased risk.
"Emergency room physicians and radiologists need effective tools like our program to quickly identify those COVID-19 patients whose condition is most likely to deteriorate quickly so that healthcare providers can monitor them more closely and intervene earlier," said first author Farah Shamout, PhD, of New York University Abu Dhabi, in a statement from the university.
Chest x-ray imaging is a first-line triage tool for COVID-19 patients. Although knowledge of COVID-19 infection is rapidly evolving, the correlation between pulmonary parenchymal patterns visible in chest x-rays and clinical deterioration remains limited. A majority of the previous work using x-ray data of COVID-19 patients has focused on diagnosis rather than prognosis, according to the authors.
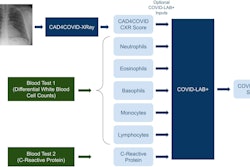
In this study, researchers developed an AI algorithm to perform an automatic evaluation of deterioration risk based on chest x-rays combined with routinely collected clinical variables. To train the model, the researchers tapped several hundred gigabytes of data gleaned from 5,224 chest x-rays acquired from 2,943 seriously ill patients infected with SARS-CoV-2 between March 3, 2020, and May 13, 2020, at NYU Langone Health.
Importantly, clinical variables known to be strong predictors of deterioration, such as the patients' age, race, and gender, along with several vital signs and laboratory test results, including weight, body temperature, and blood immune cell levels, were also factored into the AI model's predictions. Deterioration was defined as the composite outcome of one of three adverse events: intubation, admission to the intensive care unit, and in-hospital mortality.
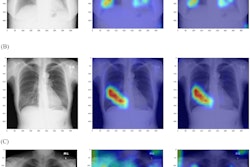
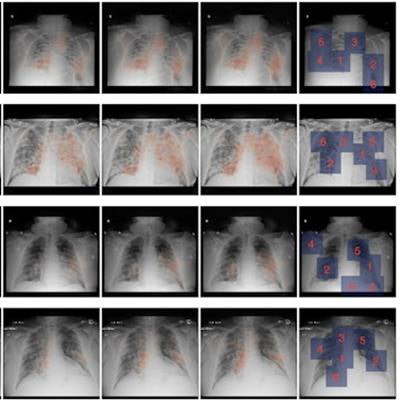
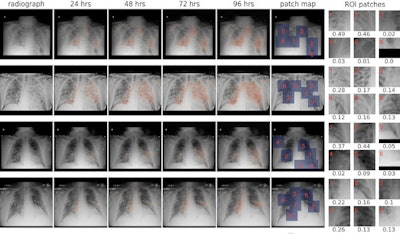 From left to right: the original x-ray image; saliency maps for clinical deterioration within 24, 48, 72, and 96 hours; locations of region-of-interest (ROI) patches; and ROI patches with their associated attention scores. All four patients were admitted to the intensive care unit and were intubated within 48 hours. Image courtesy of npj Digital Medicine.
From left to right: the original x-ray image; saliency maps for clinical deterioration within 24, 48, 72, and 96 hours; locations of region-of-interest (ROI) patches; and ROI patches with their associated attention scores. All four patients were admitted to the intensive care unit and were intubated within 48 hours. Image courtesy of npj Digital Medicine.Compared with two chest radiology experts with 20 years of experience between them, the AI algorithm accurately predicted four out of five infected patients who required intensive care and mechanical ventilation or who died within four days of admission. Temperature was ranked among the top two predictive features and age was ranked among the top four predictive features across all time windows (24, 48, 72, and 96 hours).
The researchers stated that their main finding was that the AI model achieved a comparable performance to radiologists across all time windows in terms of the area under the receiver operating characteristic curve (AUC), but outperformed radiologists for predicting a patient's deterioration at 48, 72, and 96 hours. For example, the model achieved AUC of 0.808, compared with the average AUC of 0.741 of both radiologists in the 96-hour prediction task.
"The system aims to provide clinicians with a quantitative estimate of the risk of deterioration, and how it is expected to evolve over time, in order to enable efficient triage and prioritization of patients at high risk of deterioration. The tool may be of particular interest for pandemic hotspots where triage at admission is critical to allocate limited resources such as hospital beds," the authors wrote.
The long-term goal is to deploy the system in existing clinical workflows to assist clinicians and assess whether chest x-rays contain useful information for survival analysis, they added.
Shamout and colleagues noted that although pulmonary disease is the main complication associated with COVID-19, poor outcomes are also associated with nonpulmonary complications, such as stroke and pediatric inflammatory syndromes. However, incorporating other types of data into the model could further improve its prognostic accuracy, they suggested.
"We anticipate that such tools will play an increasingly important role in supporting clinical decision-making in the future," the researchers concluded.