
Providing patient decision aids (PDAs) could reduce lawsuits in interventional radiology resulting from inadequate informed consent conversations, according to a study published September 21 in the American Journal of Roentgenology.
A group at Stanford University studied the impact of PDAs among patients undergoing informed consent conversations for outpatient image-guided procedures. Patients who received a two-page PDA before their visit reported significantly greater understanding of the procedure and its benefits, risks, and alternatives, the team found.
"Inadequate periprocedural communication is a common source of malpractice claims," wrote corresponding author Dr. Eric Keller, a vascular and interventional radiology resident, and colleagues.
Multiple studies have suggested that consent practices are limited in completeness and consistency, with information often presented in a manner beyond the health literacy of decision-makers. These limitations in the consent process present ethical concerns, according to the authors.
Moreover, inadequate communication prior to procedures is a common source of dissatisfaction and medical errors, and a precursor to lawsuits, they wrote.
One well-supported means of improving consent practices is to use PDAs. These decision aids are educational materials (handouts, videos, or other media) that present balanced information about the benefits, risks, and alternatives of a healthcare decision.
To explore the impact of PDAs on understanding and satisfaction among patients, the researchers enrolled 105 patients scheduled for visits to two academic interventional radiology clinics. The PDAs covered seven procedures: kidney ablation, liver ablation, lung ablation, inferior vena cava filter removal, transarterial chemoembolization, transarterial radioembolization, and uterine fibroid embolization.
Fifty-three patients were emailed PDA attachments about their procedures, and 52 did not receive PDAs. Patients then completed a postvisit survey (phone or online) assessing their understanding of the procedure and satisfaction with the consent conversation.
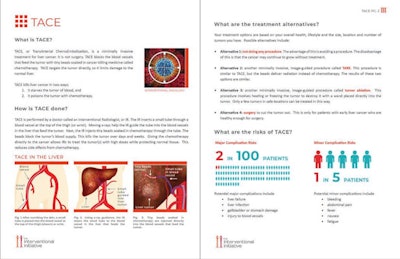 Example of a patient decision aid for transarterial chemoembolization (TACE). Image courtesy of the American Journal of Roentgenology.
Example of a patient decision aid for transarterial chemoembolization (TACE). Image courtesy of the American Journal of Roentgenology.According to the findings, patients who received a PDA compared with those who did not reported a significantly greater understanding of what the procedure involves, as well as of the procedure's benefits, risks, and alternatives.
In addition, patients who received a PDA were more likely to feel that their doctor spent enough time with them, listened carefully, provided enough time to make a decision, encouraged them to ask questions, and answered all of their questions.
Finally, patients who received a PDA, compared with those who did not, showed overall greater satisfaction with the discussion and the information provided, although this difference was not statistically significant (9.6 vs. 9.3, p < 0.06), the researchers found.
"The findings indicate an approach to incorporating PDAs into clinical workflows that can enhance patients' sense of empowerment in making decisions about their care," the authors wrote.
Importantly, the researchers noted that although studies suggest consent practices are often limited by time constraints and variable health literacy among patients, benefits were achieved in this study despite not requiring any additional time or effort by the clinicians performing the consent conversations.
The authors also noted that a majority of PDAs currently available for image-guided procedures are limited in quality, with poor readability scores and language that is above the average health literacy level. The findings of this study illustrate the need to develop well-vetted and validated PDAs that are written at the CDC's recommended 6th-8th grade health literacy level, they wrote.
"Future investigations are warranted to assess the impact of PDAs in different clinical settings and patient populations, as well as to explore workflows for PDA administration that contribute to sustained adoption," Keller and colleagues concluded.




















