CHICAGO - A commercially available artificial intelligence (AI) algorithm approved for detecting bone fractures showed high sensitivity in osteoporosis patients with suspected vertebral fractures, yet appears limited in mild cases, according to research presented at RSNA 2022.
In a scientific session on spine imaging, Dr. Jonas Oppenheimer of the Charite - Berlin University of Medicine in Germany presented results of a study testing the performance of BoneView (Gleamer, France) for detecting vertebral fractures in osteoporotic patients compared with the standard clinical method used by radiologists. They found the AI software showed a high specificity for profound vertebral fractures, yet low sensitivity for slight compression fractures.
"As muskuloskeletal radiologists, these are probably something we see every day, and subtle vertebral compression fractures are easily missed in plain-film radiographs," Oppenheimer told attendees.
Gleamer's BoneView was approved by the U.S. Food and Drug Administration in March 2022 for detecting fractures on x-rays, and previous research suggests the algorithm can significantly improve radiologist performance, particularly in trauma patients.
Oppenheimer noted that fracture detection in lumbar spine radiographs in osteoporotic patients poses unique challenges due to the presence of multiple fractures of different severity and ages, severe degenerative changes of the spine, and previous surgical interventions.
To the test whether the software might aid radiologists in these cases, the researchers compared its performance in a per vertebrae analysis compared with the standard clinical Genant classification method, which clinicians use to grade vertebral fractures from normal to severe on a scale of zero to three.
Oppenheimer and colleagues included lumbar spine radiographs from 60 osteoporotic patients with suspected fractures. The presence and Genant grade of fractures (1-3 by percentage of height loss) was defined by written reports by a radiologist with eight years of experience in muskuloskeletal imaging. The x-ray images were then analyzed by the AI software, which identified vertebras as definitely or likely fractured, and a per vertebrae comparison of AI classification to Genant grade was performed.
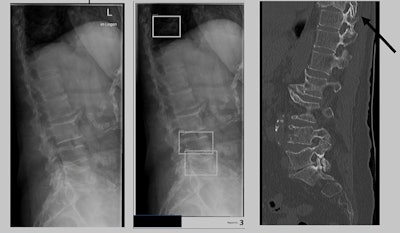 Examples of x-ray images used in the study, with boundary boxes shown by the AI software around areas of suspected vertebral compression fractures. Image courtesy of Jonas Oppenheimer.
Examples of x-ray images used in the study, with boundary boxes shown by the AI software around areas of suspected vertebral compression fractures. Image courtesy of Jonas Oppenheimer.Thirty patients had at least one fracture, with a total of 62 vertebral fractures in 435 analyzed vertebrae. Thirty fractures were labeled by the radiologist as Genant grade 1, 20 were grade 2, and 12 were classified as grade 3. For detecting and classifying these fractures, the overall sensitivity of the algorithm was 79%, with a sensitivity of 66.7% for grade 1, 90% for grade 2, and 91.7% for grade 3. The specificity of the algorithm was 96%.
While the sensitivity of the algorithm is high for more profound compression fractures, the value of this may be tempered by the fact that these fractures are also easily detected by radiologists, Oppenheimer said. Moreover, four images in severely obese patients were rejected by the algorithm, which misclassified them as abdominal radiographs.
"AI software may aid in detection of these fractures; however, it shows limited performance for Grade 1 fractures," Oppenheimer concluded.