A group in Australia has developed an AI model that shows promise in predicting fracture risk in patients based on dual-energy x-ray absorptiometry (DEXA) exams, according to a study published October 19 in JBMR Plus.
The goal is to develop AI that could serve as a screening tool, wrote lead author Damith Senanayake, PhD, of the University of Melbourne, and colleagues.
“Accurate prediction of fracture events could trigger prompt preventive strategies, which have demonstrated to be effective in reducing the number of events and their devastating consequences,” the researchers wrote.
DEXA scans are one of the most frequently used imaging techniques for calculating bone mineral density (BMD) and the current gold standard for diagnosing osteoporosis. However, calculating fracture risk using DEXA image features is rarely performed due to the complex data analysis required. Rather, clinicians often base risk on whether people have experienced falls, the researchers noted.
Thus, the aim of this study was to employ AI technology together with DEXA images and patient clinical information to evaluate fracture risk in a group of fallers and age-matched healthy controls.
Notably, the researchers employed a relatively new approach. They combined a vision transformer (ViT) model with a standard convolutional neural network (VGG-16 and Resnet-50). These technologies emerged separately as ways to identify, classify, and segment objects in images. Evidence now suggests that they are more powerful used together than either approach used alone, the group wrote.
For data, the researchers gathered whole-body DEXA images, as well as isolated images of the hip, forearm, and spine (1,488 in total), from 478 fallers and 48 non-faller controls. Model input included osteoporosis landmarks on the scans, BMD measurements of the hip and lumbar spine, as well as clinical variables, such as vitamin D and calcium levels.
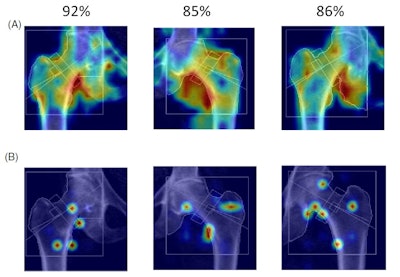 Visualization of EigenGradCAM (A) and GradCAM results (B) illustrating association between fracture group classification and DXA image features for moderate fracture risk subjects. Given are the three highest confidence images with labels predicted for correct classifications, which ranged from 85%
Visualization of EigenGradCAM (A) and GradCAM results (B) illustrating association between fracture group classification and DXA image features for moderate fracture risk subjects. Given are the three highest confidence images with labels predicted for correct classifications, which ranged from 85%
to 92% confidence. Image courtesy of JBMR Plus.
The researchers split the complete dataset into two random groups of data, a set comprising 90% of the images to train the model, and a hold-out test set with the remaining 10% of the images. The assessment was based on the model’s accuracy for classifying low, moderate, or high risk of fractures on the imaging.
According to top-line results, the model correctly classified risk with an average area under the receiver-operating characteristic curve score of 74.3%.
Ultimately, the study shows that artificial neural networks, together with DEXA images and patient clinical data in fallers, can be used to classify fracture risk with high levels of accuracy, the researchers wrote.
Additional research is warranted, they noted.
“In future research, larger high-resolution image datasets may further improve fracture risk assessment and provide scope for gradient-based class activation maps for identifying image-based regions of interest on DEXA scans that are indicative of fracture risk,” the group concluded.
The full article is available here.