A fluoroscopy method incorporating a noncontrast x-ray pulsatility index (XPI) can improve clinical efficiency as a screening or diagnostic test for suspected chronic thromboembolic pulmonary hypertension, according to research presented at the American Roentgen Ray Society (ARRS) annual meeting.
In a May 7 online presentation, Matthew Smith, MD, from Vanderbilt University Medical Center in Nashville, TN, described how the fluoroscopic XPI method could be a suitable alternative to pulmonary angiography in evaluating and monitoring pulmonary blood flow.
“Additionally, this easy-to-implement method can be performed by an x-ray technologist in an outpatient setting,” Smith said.
Time-dependent x-ray attenuation sends signals that aren’t constant, but rather oscillate around the same frequency as the heart rate. Smith said that this could make way for evaluating pulmonary blood flow without iodinated contrast using fluoroscopy.
“X-ray signal oscillation comes from vessel compliance during the cardiac cycle,” he explained. “When vessel diameter increases during the systole, more x-rays are attenuated.”
Smith and colleagues compared the perfusion map obtained without contrast using spectral analysis with the clinical gold standard of pulmonary angiography. For their prospective study, the researchers enrolled volunteers suspected of chronic thromboembolic pulmonary hypertension based on pulmonary scintigraphy and/or CT angiography (CTA).
The team performed fluoroscopic acquisition (70 kV, 30 frames/s) over an eight-second breath hold in either the right or left anterior oblique for the lungs. It also used the Fourier transform method to break down temporal signals from each pixel into individual frequency components.
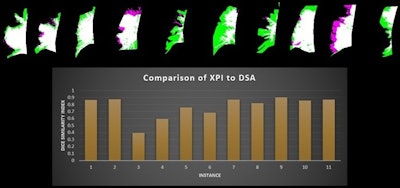 Dice similarity index measurements compare the x-ray pulsatility index (XPI) to digital subtraction angiography in patients with suspected chronic thromboembolic pulmonary hypertension. XPI is green, pulmonary angiography is pink and the overlap between the two is white. Image courtesy of the ARRS.
Dice similarity index measurements compare the x-ray pulsatility index (XPI) to digital subtraction angiography in patients with suspected chronic thromboembolic pulmonary hypertension. XPI is green, pulmonary angiography is pink and the overlap between the two is white. Image courtesy of the ARRS.
From there, the researchers isolated heart rate signal oscillation using a band-pass filter and amplitude XPI mapped to form an image. They also performed digital subtraction pulmonary angiography immediately following each fluoroscopic acquisition for spectral analysis. They did so with catheter-injected contrast in the same projection using standard protocols. Finally, the researchers segmented perfusion maps by using a blinded manual technique, as well as a semiautomated threshold and region-growing method.
Noncontrast (XPI) and contrast pulmonary angiography images were obtained in 11 different lungs. The team reported that all patients were able to perform satisfactory breath hold, despite moderate to severe disease. In addition, all patients were able to perform a satisfactory breath hold, despite moderate to severe disease.
A comparison of segmentation maps showed an average Dice score of 0.77, suggesting “excellent” agreement between XPI and pulmonary angiography maps in picturing regions of blood flow and lack of blood flow.
Smith and co-authors highlighted that this method may also lead to financial benefits and improved patient satisfaction, citing higher costs and increased waste and workflows associated with angiography. They also indicated that future work will focus on developing a clinical perfusion scoring system.
The scientific poster was awarded with ARRS annual meeting cum laude honors.