Dark-field x-ray imaging can provide insights into bone microstructure and could potentially have a role in assessing osteoporosis, according to a study published November 4 in European Radiology Experimental.
In a study using human cadaveric vertebrae, a team of researchers in Munich, Germany, found significant correlations between dark-field signals and microstructure bone parameters measured by CT.
“This finding implies the potential application of dark-field imaging to draw conclusions on bone microstructure for predicting bone stability at a lower radiation exposure than in tomographic modalities,” wrote Jon Rischewski, a doctoral candidate at Ludwig Maximilian University of Munich, and colleagues.
Osteoporosis is a systemic bone disease defined by low bone mass and the deterioration of microstructural skeletal tissue (trabecular bone tissue), and results in an increased risk of fractures. Quantitative CT measurements can be used to screen for the disease.
Dark-field imaging -- which measures ultra-small-angle scattering that takes place at material interfaces within targets -- has so far mainly been investigated for use in pulmonary imaging. Recently, however, the group showed the feasibility of using the technology to distinguish between osteoporotic from non-osteoporotic spine samples, and in this study they sought to carry the work forward another step.
The group harvested a total of 35 human cadaveric lumbar vertebrae (L2–L4) from 12 donors (7 females, 5 males) within 24 hours after death; 14 were classified as osteoporotic/osteopenic and 21 as non-osteoporotic/osteopenic. The donors' average age was 68.5 years old; the average weight was 86.1 kg, and average body mass index was 31.3 kg/m2.
The investigators obtained both vertical and horizontal dark-field images. A larger distance was required between the bone sample and the x-ray beam than in previous pulmonary patient studies to increase the dark-field signal sensitivity for osseous structures, they noted. The team reduced potential effects of air around the samples by scanning the specimen in a water bath.
The researchers used standard micro-CT to measure bone microstructural parameters such as trabecular number, trabecular thickness, bone volume fraction, and degree of anisotropy. They used spectral CT to measure hydroxyapatite density and then analyzed correlations among the CT and dark-field imaging findings.
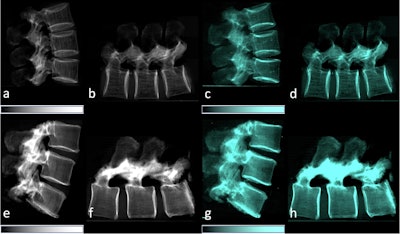 Lateral conventional attenuation (a, b, e, f) and co-registered dark-field (c, d, g, h) images of two spine specimens. Vertical (a, c, e, g) and horizontal (b, d, f, h) scans of the spine specimen of a 77-year-old female with osteoporosis (bone mineral density = 65.75 mg/dL) (a–d) and a non-osteoporotic spine specimen (e–h) of a 61-year-old female (bone mineral density = 169.38 mg/dL).Image available for republishing under Creative Commons license (CC BY 4.0 DEED, Attribution 4.0 International) and courtesy of European Radiology Experimental.
Lateral conventional attenuation (a, b, e, f) and co-registered dark-field (c, d, g, h) images of two spine specimens. Vertical (a, c, e, g) and horizontal (b, d, f, h) scans of the spine specimen of a 77-year-old female with osteoporosis (bone mineral density = 65.75 mg/dL) (a–d) and a non-osteoporotic spine specimen (e–h) of a 61-year-old female (bone mineral density = 169.38 mg/dL).Image available for republishing under Creative Commons license (CC BY 4.0 DEED, Attribution 4.0 International) and courtesy of European Radiology Experimental.
The team found that the dark-field signal was significantly lower in the osteoporotic/osteopenic vertebrae compared to non-osteoporotic/osteopenic samples for both the vertical and horizontal orientation, and it correlated significantly with the CT measurements.
Specifically, the researchers found a significant positive correlation between the dark-field signal from the vertical position with trabecular number (p = 0.005), bone volume fraction (p = 0.007), degree of anisotropy (p = 0.01), and hydroxyapatite density (p = 0.01).
In addition, the calculated ratio of the vertical/horizontal dark-field signal also correlated significantly with trabecular number (p = 0.011), bone volume fraction (p = 0.032), degree of anisotropy (p = 0.002), and hydroxyapatite density (p = 0.049).
“Utilizing a prototype clinical x-ray dark-field radiography system, we observed a significant correlation between the dark-field signal and microstructure bone parameters of vertebral trabecular bone,” the group wrote.
Ultimately, bone strength is highly determined by bone microstructure and micro-CT imaging is among the most detailed approaches for assessing microstructure, the authors noted. However, the approach can only be applied in an ex vivo setting due to setup constraints and high radiation doses, they added.
Conversely, as has been shown in lung studies, dark-field radiography exposes patients to significantly lower radiation, they wrote.
“Dark-field imaging could, therefore, be a useful tool for assessing microstructural alterations of bone and become an important diagnostic component in osteoporosis imaging,” the group concluded.
The full study is available here.