If, like Dr. Harry Agress Jr., you’ve performed more than 2,000 FDG-PET imaging exams in the past few years, chances are you know something about building a successful PET practice.
As the nuclear medicine chief at the 600-bed Hackensack University Medical Center (HUMC) in New Jersey, Agress spearheaded the development of the facility’s PET services. He started out in May 1999, performing 480 coincidence detection studies with a gamma camera. After upgrading to a dedicated PET scanner in April 2000, PET imaging services took off.
The key to running a PET center with legs is to bring the referring physicians on board. Effective marketing and professional outreach are just some of the elements Agress used to make HUMC’s PET center a success. He shared his knowledge of how to promote a PET imaging center at the 2002 Society of Nuclear Medicine (SNM) meeting in Los Angeles last month. He outlined an 11-point plan that he has developed to offer PET services at his institution.
Getting educated
Education -- for you, for your technologists, and for referring physicians -- is crucial to implementing PET successfully, Agress said. Visits to an existing PET site are recommended, as is participating in tutorials such as those offered by the SNM PET Learning Center for both physicians and technologists. Keeping up with journals such as Seminars in Nuclear Medicine, the Journal of Nuclear Medicine, Radiology, Molecular Imaging and Biology, and the Journal of Clinical Oncology is also important, he said.
"At the beginning, I believe it is incredibly important for one person to be tasked with reading all the PET scans. Once they reach a level of expertise, they can teach others in the practice how to interpret the studies," Agress said.
Educating others
Having relevant PET journal articles and abstracts readily available can help educate referring physicians, Agress said. (See bibliography below.)
"When you introduce PET to a group of physicians who are used to thinking in terms of CT, MR, and tumor markers, unless they have been well-educated at their own meetings, there is a tremendous amount of resistance. It literally takes a one-on-one effort to win them over," he said.
Resistance
"I was sort of surprised at the level of resistance I encountered when I first started. I can’t emphasize enough that this is a big, big change. Oncologists are very specific, very serious, and they need proof of things. They can’t go ahead and give toxic radiation and toxic chemotherapy without knowing what’s going on. You’re completely changing the way they’re going to do something, and they really need to trust you," Agress said.
Being patient and working with physicians on a one-on-one basis will go a long way toward mitigating resistance to PET imaging. Agress strongly emphasizes that the radiologist reading PET take the time to personally go over cases with referring physicians, oncologists, and surgeons to demonstrate the power of the modality.
Presentations
Keeping, and showing, relevant cases tailored for clinical specialties can be a powerful tool when first introducing PET to referring physicians. Using a facility’s PACS to do side-by-side comparison of PET to other modalities can help win over recalcitrant clinicians, Agress said. If a PACS is not available, store the images and use a desktop presentation program, such as Microsoft PowerPoint, to display cases, he noted.
"Give presentations, go to tumor boards, go to specialty meetings, certainly give grand rounds; that’s what stimulated me to go into PET imaging three years ago," Agress said.
Initial cases
Be sure to get clinical and pathological correlations for any cases that are presented to bolster the utility of PET. When you do present, it’s vital that you emphasize the limitations as well as the positive aspects of PET, he said.
"You want to pick cases where PET imaging made a clear impact in patient management. These are cases where PET changed the outcome," Agress said.
Staffing
Setting up your facility to be successful from the start is a lot easier than changing processes and procedures when exam volume rises. To this end, HUMC has a policy of having all clinical and insurance forms filled out prior to approving and scheduling PET scans. By getting the paperwork out of the way before the patient arrives at the center, it makes the throughput that much easier.
Agress also got the HUMC administration to set up a separate phone line for the PET center and approve a dedicated PET receptionist and coordinator for exams. By doing so, patients and referring physicians experience a level of psychological comfort that they have a pipeline to the PET center.
"Probably the biggest single oversight that I made when I started was that I underestimated the time commitment involved with PET. I thought it was something like a sophisticated gallium scan. And nothing could be further from the truth. PET is a major time commitment on the part of the physician in charge and the staff," Agress said.
It’s nearly impossible to have a successful PET operation without hiring additional personnel. An experienced nuclear medicine technologist will be needed to perform exams, as well as train other technologists in the practice. Paperwork associated with PET exams is tremendous, and time to handle it needs to be factored into staffing calculations.
"You have to be prepared from day one to handle your desired volume of cases. Because once it clicks, PET imaging can take off -- and if you want to be successful, you better be ready to handle it," Agress noted.
Public relations
Agress recommends sending a letter announcing the service to all medical staffs in the region letting them know that a PET service will be in place. It’s not good that they first read about it in the paper or hear about it on the local newscast, Agress said.
Once your letter has been sent, though, you’ll want to put out press releases to the local newspapers announcing the service. PET has cachet, and if your practice is the first in the area to offer the modality, it is a newsworthy event.
Your group should also contact local radio and television outlets and offer to provide their reporters with guided tours of the facility, as well as provide them with access to the radiologist who will be interpreting the PET studies. The radiologist should be aware that most reporters know little about medical imaging and even less about PET, and thus should be careful to only say what they want to see in print, Agress cautioned.
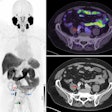
Image correlation
The CT or MR study that initiated the PET request should be read before the PET study is performed. In fact, HUMC will not perform a PET scan at its facility unless the radiologist has seen these images beforehand.
Afterward, the PET studies should be read along with the CT or MR study that initiated the PET exam, to ensure an accurate evaluation. In addition, the diagnostic report should reflect this consultative approach, correlating findings with those of all the images that sparked the PET study, according to Agress.
"Whenever I find an unusual finding, I always make a personal phone call to the referring doc," he said. "PET is a much more personally involving thing for the nuclear medicine physician or radiologist than a lot of other tests that we do."
Problems
To mitigate possible problems at the PET center, the facility’s staff sends out an information sheet that patients fill out before being scheduled for an exam. The flyer advises patients to eat a high-protein, no-carbohydrate meal the night before, drink plenty of water, avoid sugar for 24 hours before the procedure, and not eat anything after midnight the day before the exam.
All insurance paperwork for the patient is pre-checked and certified before the exam is scheduled to handle any billing issues that could arise. Patients are also advised about the physical setup of the PET scanner in order to help calm the fears of those individuals who may be affected by claustrophobia.
Follow-up
The key to developing confidence and credibility in the modality with clinicians is to follow up each PET exam with the physician who ordered it, Agress believes.
"The single most important thing is the follow up. We’ve really gotten really tenacious and compulsive about this," he said. "If you’re going to make PET an interesting thing for you, you really need to follow these cases. It’s really changed my whole practice now that I’m much more involved in the follow up."
Perseverance
Agress calls all the referring physicians within a month of performing the exam to correlate his findings. If there is a complaint about a false-positive or false-negative PET reading, he will request tissue findings and any additional images that may have been performed to verify the complaint. The majority of the time, the PET findings are proven to be correct.
"I think success with a PET center requires that you think of this as a small business, as opposed to just doing another scan," Agress said. "It requires persistence and a commitment to change in many small steps while always keeping a clear vision of the desired outcome."
By Jonathan S. BatchelorAuntMinnie.com staff writer
July 15, 2002
General PET oncology
PET Imaging in Oncology, Seminars in Nuclear Medicine, July 2000: Vol. 30:3, pp. 150-185.
Oncological Applications of FDG-PET Imaging, JNM, October 1999, Vol. 40:10, pp. 1706-1715.
PET: The Merging of Biology and Imaging into Molecular Imaging; JNM, April 2000, Vol. 41:4, pp. 661-681.
Solitary pulmonary nodules
Prospective Investigation of Positron Emission Tomography in Lung Nodules (PIOPILN); Journal of Clinical Oncology, March 1998, Vol. 16, pp. 1075-1084.
Positron Emission Tomography in Lung Cancer; Annals of Thoracic Surgery, June 1998, Vol. 65, pp. 1821-1829
General lung PET and staging
PET in Lung Cancer; JNM, May 1999, Vol. 40, pp. 814-820.
Staging Non-Small Cell Lung Cancer with Whole-Body PET; Radiology, September 1999, Vol. 212, pp. 803-809.
Staging Non-Small Cell Lung Cancer by Whole-Body Positron Emission Tomographic Imaging; Annals of Thoracic Surgery, December 1995, Vol. 60, pp. 1573-1581.
Colon carcinoma
Impact of 18F-FDG PET on Managing Patients with Colorectal Cancer: The Referring Physician’s Perspective; JNM, April 2001, Vol. 42, pp. 586-590.
Whole-Body PET Imaging with [18-F] Fluorodeoxyglucose in Management of Recurrent Colorectal Cancer; Archives of Surgery, May 1999, Vol. 134, pp. 503-511.
Staging Recurrent Metastatic Colorectal Carcinoma with PET, JNM, August 1997, Vol. 38, pp. 1196-1201.
Esophageal carcinoma
FDG PET in Esophageal Cancer: Incremental Value over Computed Tomography; Clinical Positron Imaging, May 1999, Vol. 2, pp. 255-260.
Staging of Esophageal Cancer with 18-F Fluorodeoxyglucose Positron Emission Tomography; AJR, February 1997, Vol. 168, pp. 417-424.
Lymphoma
Effect of Whole-Body 18F-FDG PET on Clinical Staging and Management of Patients with Malignant Lymphoma; JNM, August 2001, Vol. 42, pp. 1139-1143.
2-Deoxy-2-[F-18] Fluoro Glucose Imaging with Positron Emission Tomography for Initial Staging of Hodgkin’s Disease and Lymphoma, Molecular Imaging and Biology, January 2002, Vol. 4, pp. 105-114.
Melanoma
The Impact of FDG Whole-Body Positron Emission Tomography for Managing Patients with Melanoma: The Referring Physician’s Perspective; Molecular Imaging and Biology, February 2002, Vol. 4, pp. 185-190.
PET Scanning with FDG in Patients with Melanoma: Benefits and Limitations; Clinical Positron Imaging, February 1999, Vol. 2, pp. 93-98.
Breast carcinoma
FDG-PET in Breast Cancer: A Different View of Its Clinical Usefulness; Molecular Imaging and Biology, January 2002, Vol. 4, pp. 35-45.
Impact of Whole-Body 18-F-FDG PET on Staging and Managing Patients with Breast Cancer: The Referring Physician’s Perspective; JNM, September 2001, Vol. 42, pp. 1334-1337.
Carcinoma of unknown primary
FDG PET Detection of Unknown Primary Tumors; JNM, May 2000, Vol. 41, pp. 816-822.
Gynecological oncology
Lymph Node Staging by Positron Emission Tomography in Patients with Carcinoma of the Cervix; Journal of Clinical Oncology, September 2001, Vol. 19, pp. 3745-3749.
Related Reading
New tracers, technologies propel clinical applications in PET, June 14, 2002
Mobile alternative brings PET to the door, August 14, 2001
PET brings surprises in and outside the reading room, August 9, 2001
Reimbursement drives huge growth in PET, August 7, 2001
PET procedures reach 37,000 in Q4, May 10, 2001
Copyright © 2002 AuntMinnie.com