After languishing in the clinical shadows for the last 10 years, rubidium is starting to catch the attention of nuclear medicine specialists. The radiopharmaceutical can thank the Centers for Medicare and Medicaid Services (CMS) for its revival.
CMS, as of January 1, 2006, increased the reimbursement for myocardial PET perfusion imaging involving multiple studies at rest and/or stress. The new rate of $2,484.88 more than triples the 2005 rate of $735.77.
CMS came up with the new figure by analyzing hospital claims data and splitting the ambulatory payment classification (APC) into single studies and multiple studies, similar to how it handles SPECT myocardial perfusion imaging procedures. The Society of Nuclear Medicine, the Academy of Molecular Imaging, the American Society of Nuclear Cardiology, and the CMS APC panel were among the proponents advocating the level splitting.
The new rate for rubidium is based on a small number of claims, so it may not be stable in future years, said Denise Merlino, president of Merlino Healthcare Consulting of Stoneham, MA. The 2006 radiopharmaceutical code for rubidium-based PET reimbursement is A9555 per study dose. While there has been some confusion among healthcare providers who have mistakenly used A4641 as the code, CMS is expected to clarify the appropriate code choice in the near future, Merlino said.
First reimbursementRubidium-based PET imaging initially received reimbursement in 1994, four years before FDG-PET gained approval for Medicare payment. However, rubidium was overshadowed by myocardial perfusion SPECT, a much cheaper alternative for cardiac imaging.
“This financial model has been the biggest challenge to overcome ever since,” said Jonathan Frey, director of product and clinical marketing for the Molecular Imaging division at Siemens Medical Solutions of Malvern, PA. “Just about the same time rubidium entered the fray, nuclear cardiology began to take off (with SPECT) with a price point that was significantly lower.”
Bracco Diagnostics introduced rubidium in the U.S. under the product name CardioGen-82 in the mid-1990s. However, the market economics caused the Princeton, NJ-based company put CardioGen on the back burner in terms of promotion.
Three years ago, Bracco resurrected the rubidium tracer with a new business plan, and since then the company has seen an increase in usage from 13 U.S. customers in 2003 to more than 50 as of February 2006. Approximately 54% of CardioGen users are physician practices and freestanding imaging centers, with hospitals accounting for the remaining 47%.
More facilities are expected to add rubidium-based PET to their imaging services in March because of the reimbursement hike and mounting clinical evidence that rubidium is faster and more accurate for cardiac imaging than SPECT.
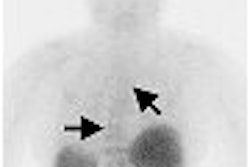
Clinical evidenceBecause rubidium has a very short physical half-life of 75 seconds, the patient must undergo pharmacological stress, and the rubidium must be injected at peak stress through an infusion system from the tracer’s generator. The generator is encased in a lead shield surrounded by a labeled plastic container.
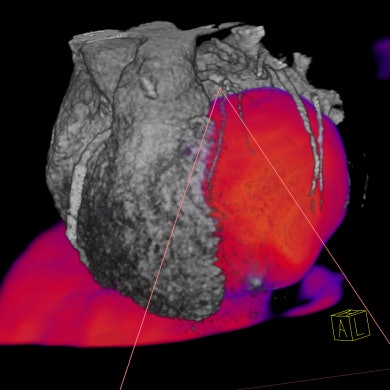 |
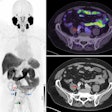
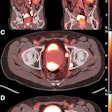
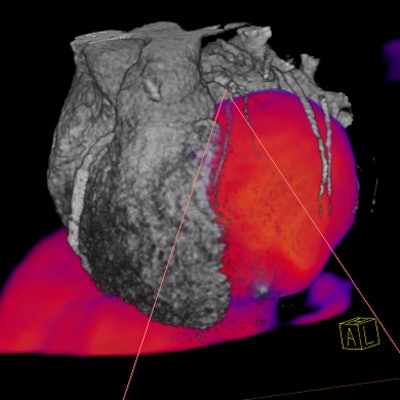
| A volume-rendered Rb-82 PET perfusion study (shown in color) fused with an automatically isolated and volume-rendered CT heart image, acquired with a Biograph PET/CT scanner. (Images courtesy of Siemens Medical Solutions, Molecular Imaging). |
To date, clinical data show that rubidium’s almost instantaneous ability to image a patient provides very high accuracy in identification of ischemia. In addition, it reduces a stress and rest test to 45 minutes, compared with routine SPECT myocardial stress imaging, which takes place over three to four hours.
“There seems to be a general consensus -- at least in the nuclear cardiology community -- that rubidium PET might replace SPECT in patients who are under pharmacological stress, simply because it is so fast,” said Dr. Marcelo DiCarli, chief of nuclear medicine and PET and co-director of cardiovascular imaging at Brigham and Women’s Hospital. DiCarli has been using rubidium for several years to build the Boston hospital’s PET program and today images between 1,100 and 1,200 cardiac patients annually with the tracer.
Rubidium-based cardiac PET has not only enhanced patient throughput with shorter scan times but has also proven beneficial for difficult-to-image patients. “Once you get into patients who are obese, we know what the limitations of SPECT are,” DiCarli said. “Those patients who need to undergo pharmacological stress are those who are usually the sickest; those are the patients for whom (rubidium-based) PET provides a significant advantage.”
Given its results with rubidium, Brigham and Women’s plans to replace one of its SPECT scanners with another PET camera in the next three to four months. “We are no longer performing pharmacological stress on SPECT,” DiCarli said. “It’s just a waste of time.”
More convertsHoly Name Hospital in Teaneck, NJ, will embark on a rubidium-based cardiac PET program in March for its chest pain protocol, offering emergency room patients a rapid assessment of myocardial viability and ischemia. Dr. Jacqueline Brunetti, medical director of radiology, sees rubidium’s potential in preoperative assessment of single- or multivessel disease, evaluation of patients’ post-therapy progress, and cardiac angioplasty.
Like any facility expanding its services, Holy Name considered the economic feasibility of establishing the program, given that the monthly cost of a rubidium generator is in the $25,000 range. A hospital or imaging center needs adequate patient volume, even with the new reimbursement rate. “There is a major expense upfront,” Brunetti said. “Having that reimbursement clearly will help generate some interest in looking at the feasibility before embarking on this type of program.”
Rubidium’s imaging accuracy is, in part, due to today’s advanced PET camera technology, which is capable of greater count rates. “From a technology perspective, the most important thing with rubidium is the ability to support a high count rate performance,” said Siemens’ Frey. “Rubidium has a very short half-life, so you are injecting fairly high quantities of dose and it is decaying very quickly. You want a fairly high count rate performance and processing software.”
Positron of Houston designed its PET scanner in the 1990s for rubidium imaging. Company president, Joseph Oliverio, who also serves as clinical supervisor for the nuclear medicine technology program at the University of Buffalo, NY, said there is a possible pitfall in rubidium’s increased reimbursement rate. While he doesn’t quarrel with the radiotracer's clinical benefits, he questioned whether third-party payors would balk at the widening reimbursement gap between PET and SPECT for cardiac imaging.
“If I go back to my insurance company and tell them it will be $700 more expensive than what we are charging now, they may limit me to one indication, and that may be only after SPECT is performed or it’s equivocal,” Oliverio said.
What’s next?
With the exponential growth in PET camera installations in the U.S. this decade, the efficacy of rubidium in cardiac PET imaging may further catalyze market growth. Although the clinical data on rubidium-based PET imaging are not abundant, Brigham and Women’s DiCarli is hoping to fill the void by participating in a clinical study to compare the diagnostic accuracy, cost-effectiveness, and prognosis of PET, SPECT, and CT coronary angiography.
“We could get the kind of data to convince payors that (rubidium-based) PET in selective patients may be the best test-of-choice,” DiCarli said. “The data also will be helpful in refining cardiology guidelines to guide people on how to use the technology in patients with (certain) conditions.”
Holy Name’s Brunetti already sees the promise of rubidium-based cardiac PET. “We are only on the crest of the wave here. Sometimes you start out with an answer in search of a question,” she said. “In this particular case, the answer is so powerful that this will be rapidly adopted in many hospitals.”
By Wayne Forrest
AuntMinnie.com contributing writer
February 23, 2006
Related Reading
PET can help heart patients avoid cardiac cath, June 21, 2005
Imaging tackles cardiac 'octopus pot' syndrome, April 19, 2005
PET Medicare reimbursement -- narrow but widening, June 17, 2004
Copyright © 2006 AuntMinnie.com