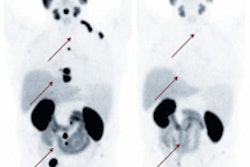
BALTIMORE - FDG-PET and FDG-PET/CT do a good job in predicting the chances of recurrence and survival for patients with head and neck cancer within two years of completing chemotherapy treatment, according to a study presented on Sunday at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
Researchers from Johns Hopkins University, led by Dr. Sara Sheikhbahaei, a postdoctoral fellow in the department of radiology and radiological sciences, found that patients with a positive PET scan were associated with a more than sevenfold increased risk of a death within two years of treatment.
The results are significant as proponents of PET/CT imaging are trying to persuade federal authorities to loosen the purse strings on reimbursement for the modality, as Medicare payments are currently limited to three follow-up PET/CT scans.
The importance of follow-up
Post-treatment follow-up is key in the management of patients with head and neck cancer, allowing clinicians to better predict efficacy of treatment and also detect recurrences that might require further treatment, Sheikhbahaei told AuntMinnie.com.
 Dr. Sara Sheikhbahaei, a postdoctoral fellow in the department of radiology and radiological sciences at Johns Hopkins University School of Medicine.
Dr. Sara Sheikhbahaei, a postdoctoral fellow in the department of radiology and radiological sciences at Johns Hopkins University School of Medicine."Until now, there has been no scientific evidence that conventional anatomic imaging can distinguish between treatment-induced inflammation or fibrosis and residual tumor," she said. "There have been previous meta-analyses that evaluated the prognostic value of a baseline or staging PET scan, but there has been no meta-analysis focusing on the predictive value of a post-treatment PET/CT scan."
Sheikhbahaei and colleagues searched Medline and Embase through November 2014 for studies in which patients received a PET/CT scan after primary chemotherapy. Survival data for two or more years as part of a patient's follow-up was collected to determine overall survival and event-free survival. Researchers reported the combined hazard ration for outcome and also performed risk-ratio assessments of overall and event-free survival after two years and between three to five years.
The researchers included 26 studies that met their inclusion criteria. Eight studies with a total sample of 549 patients addressed overall survival and produced a pooled hazard ratio of 3.81, meaning a patient with a positive PET scan had almost four times the risk of death. Seven studies with a total of 428 patients covered event-free survival and had a pooled hazard ratio of 5.43.
A positive PET scan after chemotherapy was associated with a risk ratio of 7.35 for death, meaning patients had a more than sevenfold increase in the risk of death within two years. In the longer follow-up time of three to five years, a positive PET scan had a risk ratio of 2.42 for death.
The standard practice in treating head and neck cancer is to perform a PET/CT scan 12 weeks after clinical therapy, but some of the studies in the meta-analysis evaluated PET and PET/CT scans performed during the therapy process (intratherapy).
In a review of 328 patients who received intratherapy PET or PET/CT scans, the risk ratio for death was 5.05. So patients with a positive scan were slightly more than five times more likely to die within two years. Among 384 patients who were evaluated with an intratherapy PET or PET/CT scan for head and neck cancer recurrence or progression during treatment, the risk ratio was 3.71, meaning there was an almost four times greater chance the cancer would come back or advance.
"Our results show that a positive PET/CT scan strongly predicts overall survival and event-free survival in head and neck cancer patients," Sheikhbahaei concluded. "In the group analysis, we noticed that both post-therapy and intratherapy PET/CT scans were significantly associated with survival."
Evidence-based research
The results of the meta-analysis contribute to the call for more evidence-based research to prove the diagnostic and clinical value of imaging, as advocated by SNMMI, the U.S. Centers for Medicare and Medicaid Services (CMS), and third-party payors.
 Dr. Rathan Subramaniam, PhD, associate professor of radiology and radiological science, oncology, otolaryngology -- head and neck surgery, and health policy and management at Johns Hopkins.
Dr. Rathan Subramaniam, PhD, associate professor of radiology and radiological science, oncology, otolaryngology -- head and neck surgery, and health policy and management at Johns Hopkins."Imaging is just one action of multiple actions that help determine an outcome," study co-author Dr. Rathan Subramaniam, PhD, associate professor of radiology and radiological science, oncology, otolaryngology -- head and neck surgery, and health policy and management at Johns Hopkins, told AuntMinnie.com. "We are trying to show that it is possible to link imaging to outcome. Here we are showing that if a post-therapy PET/CT scan is negative, then that patient is likely to survive much longer than if the post-therapy PET/CT was positive."
Currently, CMS pays for three post-treatment PET/CT studies as part of the subsequent antitumor treatment strategy, nationally, for a type of cancer in a patient. Further PET/CT studies are covered at the discretion of local Medicare administrators when performed for appropriate clinical context, which is necessary and reasonable for patient management.
"One of the main questions in imaging today that payors and CMS are asking is what is the value of post-treatment imaging and what is the role imaging plays in these findings," Subramaniam added. "There are many single-center studies, but we needed much more robust evidence in publishing this meta-analysis."
Johns Hopkins' researchers plan to expand their meta-analysis to assess the value of more than three FDG-PET or FDG-PET/CT scans to determine the potential outcome for a head and neck cancer patient.
"We will probably work on developing this single meta-analytic evidence in more follow-up PET/CT scans to see what the value is of PET/CT two, three, or five years down the track, especially in a clinical context," he said.