The addition of F-18 choline PET to multiparametric MRI (mpMRI) can significantly improve the detection of higher-risk primary prostate cancer and assessment of patients with suspected cases, according to a study published in the March issue of the Journal of Nuclear Medicine.
Choline-PET greatly increased the accuracy of mpMRI alone to identify prostate cancer rated as Gleason 3 and 4, and it eliminated the need for an unnecessary biopsy among patients with lower-risk forms of the disease.
"Our data indicate that in the future, patients with elevated prostate cancer risk might undergo F-18 choline PET/mpMRI rather than mpMRI alone, followed by confirmatory histologic sampling only if PET/mpMRI suggests the presence of significant disease," wrote the authors, led by Dr. Matthew Davenport from the radiology department at the University of Michigan (JNM, March 2020, Vol. 61:3, pp. 337-343). "This diagnostic approach not only improves detection of clinically significant prostate cancer and decreases the number of unnecessary prostate biopsy procedures but also ... is cost-effective."
Where mpMRI falls short
Clinicians increasingly are turning to mpMRI to detect and assess the extent of primary prostate cancer and to more "cost-effectively identify a significantly greater fraction" of more severe cases, the authors noted. "These outcomes are important because accurate risk stratification of primary prostate cancer has been fraught with overdiagnosis and overtreatment."
Even with its ability to help determine which patients need biopsy and subsequent treatment, mpMRI also produces a greater number of false positives, achieves only moderate interrater agreement, and requires a "steep learning curve, each contributing to unnecessary biopsies that drive complication rates and unwanted detection of low-risk disease," Davenport and colleagues added.
Given PET's prowess in oncologic imaging, it seemed a natural choice to add the modality to mpMRI to improve the detection and evaluation of suspicious prostate cancer cases. In fact, a June 2019 study, led by current study co-author Christine Barnett, PhD, senior research health economist with RTI Health Solutions, used nine different screening scenarios to conclude that F-18 choline PET with mpMRI was more cost-effective than mpMRI alone.
They found that the combination greatly reduced the number of unwarranted biopsies by determining which men with elevated prostate-specific antigen levels did not need the procedure.
Risk stratification
In this prospective single-center clinical trial, Davenport, Barnett, and colleagues sought to advance their previous research by investigating whether choline-PET could improve the accuracy of mpMRI for patients with Gleason prostate cancer scores of 3 and 4 and determine the need for a prostate biopsy.
The researchers analyzed 56 patients who underwent 3-tesla MRI scans of the pelvis (Ingenia, Philips Healthcare) with a protocol that included axial 2D and 3D T2-weighted fast spin-echo imaging, axial diffusion-weighted imaging, and axial T1-weighted unenhanced and dynamic contrast-enhanced MRI. Images were prospectively classified on the five-point Likert scale, with a score of 1 indicating a negative result for cancer and 5 as positive for cancer. Likert scores of 1 and 2 were not referred for a biopsy, while scores of 3, 4, and 5 were targeted for follow-up biopsy.
The subjects also underwent choline-PET/CT imaging (Biograph TrueV mCT, Siemens Healthineers), with the PET portion scanning the lower abdomen and pelvis 20 minutes after injection of 230 (± 31 MBq) of choline. A choline tumor-to-background ratio (TBR) of 1.58 or greater was a positive indication for cancer.
Biopsies were performed on average 17.8 days (± 14.9 days) after PET or mpMRI using a navigated 3D ultrasound system (Logiq E9, GE Healthcare). A total of 224 targeted and 672 standard biopsy cores were obtained. The biopsies confirmed 27 Gleason 3 and 4 cancers in 24 subjects (43%).
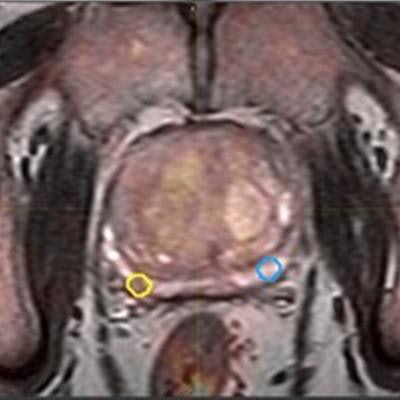
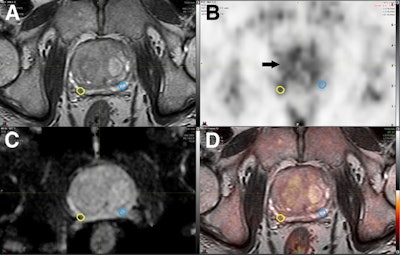 The images show coregistered axial 3D T2-weighted fast spin-echo MRI (A), choline-PET (B), apparent diffusion coefficient map (C), and PET/mpMRI (D). A small 0.16 cm3 right peripheral zone intermediate risk lesion (yellow circles) was confirmed as Gleason 4 + 4 cancer. Respective mirrored background volume of interest (blue circles) is shown, resulting in choline TBR of 1.61. Diffusely increased choline uptake is noted in benign prostate hyperplasia (arrow). Images courtesy of the Journal of Nuclear Medicine.
The images show coregistered axial 3D T2-weighted fast spin-echo MRI (A), choline-PET (B), apparent diffusion coefficient map (C), and PET/mpMRI (D). A small 0.16 cm3 right peripheral zone intermediate risk lesion (yellow circles) was confirmed as Gleason 4 + 4 cancer. Respective mirrored background volume of interest (blue circles) is shown, resulting in choline TBR of 1.61. Diffusely increased choline uptake is noted in benign prostate hyperplasia (arrow). Images courtesy of the Journal of Nuclear Medicine.Modality accuracy
As for mpMRI alone, the modality prospectively identified 90 lesions prior to biopsy, of which there were 40 low-risk lesions (44%) (Likert 3), 30 intermediate-risk lesions (33%) (Likert 4), and 20 high-risk lesions (22%) (Likert 5). On that per-lesion basis, mpMRI overall achieved accuracy of 68% for Likert 3, 4, and 5 lesions.
The researchers then analyzed several choline-PET/mpMRI models and found the most effective approach for prostate cancer detection was to combine low- (Likert 3), intermediate- (Likert 4), and high-risk (Likert 5) mpMRI results with an elevated choline TBR greater than 1.58 as positive for significant cancer.
This combination increased accuracy on a per-lesion basis significantly to 89% (p < 0.001). In fact, the choline TBR threshold of 1.58 significantly improved the diagnostic accuracy over the mpMRI on a per-patient basis, as well, from 87% to 93% (p < 0.001).
"In a hypothetical future state, patients with elevated prostate cancer risk might undergo choline-PET/mpMRI rather than mpMRI alone, followed by confirmatory histologic sampling only if PET/mpMRI suggests the presence of significant disease," the researchers concluded.