Blood tests that detect a biomarker for abnormal tau metabolism in the brain were able to detect pathology earlier than PET scans in patients with preclinical Alzheimer's disease (AD) in a study reported online November 9 in JAMA Neurology.
The study of 490 people included healthy controls and participants with subjective cognitive decline or mild cognitive impairment who were tested for tau phosphorylated at threonine 217 (p-tau-217). Various methods of early detection of Alzheimer's were compared for their value in the detection of preclinical disease.
"In this cohort study, plasma [p-tau-217] levels were increased during the early preclinical stages of AD when insoluble tau aggregates were not yet detectable by tau-PET," reported a group led by Shorena Janelidze, PhD, of the Clinical Memory Research Unit at Lund University in Sweden. "Plasma [p-tau-217] may hold promise as a biomarker for early AD brain pathology."
The data reported in JAMA Neurology derive from a cohort of the Swedish BioFINDER (Biomarkers for Identifying Neurodegenerative Disorders Early and Reliably) study. At the Alzheimer's Association International Conference in July, researchers with BioFINDER-2, which is partly supported by Eli Lilly, reported that plasma p-tau-217 was effective for discriminating Alzheimer's disease from other neurodegenerative conditions, with better performance than p-tau-181, neurofilament light chain, and other biomarkers.
The data just reported in November compared p-tau-217 with cerebrospinal fluid (CSF) and PET biomarkers at the very earliest disease stages. A blood test for early Alzheimer's disease promises to be more cost-effective as well as less invasive than CSF and PET -- important goals for research and development as well as for treatment. Diagnosing dementia diseases decades before symptoms become apparent is a dream researchers believe can be achieved with the help of blood testing.
Janelidze and colleagues' analysis included 225 healthy controls, 89 with subjective cognitive decline, and 176 with mild cognitive impairment. All of the participants, who were studied at two different hospitals in Sweden, had blood and CSF testing for p-tau-217, as well as PET imaging for beta-amyloid and tau pathology.
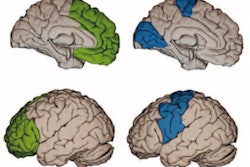
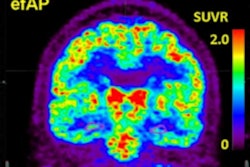
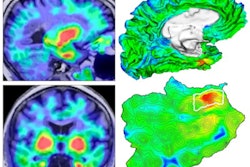
Plasma and CSF p-tau-217 testing were performed by Lilly researchers on the company's Meso Scale Discovery immunoassays. For PET imaging, beta amyloid was assessed with flutemetamol F-18 (Vizamyl, GE Healthcare) and tau was measured with Roche's RO948 F-18 radiotracer. At the earliest stages of Alzheimer's disease in people who are not cognitively impaired, tau pathology is found in the entorhinal cortex, and researchers focused on PET signals in this region.
In participants who were not cognitively impaired and had abnormal beta amyloid on PET but were negative for tau pathology with the modality, plasma p-tau-217 levels were elevated, researchers noted (median increase of 2.2 pg/mL). Furthermore, plasma p-tau-217 was significantly correlated with CSF p-tau-217 in those who were not cognitively impaired and also beta-amyloid positive on PET. And an event-based modeling analysis indicated that p-tau-217 on both plasma and CSF would change earlier than signals on tau-PET.
Along with other datasets, the report serves as proof of concept for the idea that blood tests for beta-amyloid and tau pathology are "essentially equivalent to that of CSF or PET," wrote Elisabeth Thijssen and Dr. Gil Rabinovici, both of the Memory and Aging Center at the University of California, San Francisco in an accompanying editorial.
However, while there is cause for optimism and excitement, it's also important to acknowledge that most use of blood tests to date has been in academic and industry research labs, so real-world performance still needs to be evaluated, they wrote in the editorial, which was also published November 9 in JAMA Neurology.
"It seems like only a matter of time before a panel of blood tests will be widely available to assess [amyloid, tau, and neurodegeneration] brain changes in research and in the clinic, transforming the diagnosis and care of patients in the earliest stages of AD," Thijssen and Rabinovici wrote.