SmithGroup, Inc.
Medical imaging sites are by far the most complex facilities in healthcare, and among imaging sites, MRI facilities are often the most intricate and multifaceted, with myriad design and operational elements requiring careful integration.
Nowhere else is both the healthcare provider and designer faced with such diverse issues of physics, workflow, aesthetics, weight, safety, and economics. Each of these requirements must be satisfied without compromising any of the others. Given the rate at which MRI technology advances, future flexibility is as important as designing for initial use.
Consider also the growth of MRI as an interventional and research tool -- one that may coexist in the surgical suite, the catheterization lab, or the angiography suite -- and each of those respective environmental design requirements must be looked at in addition to multiple MRI design issues.
MRI facilities come in many sizes. Some are small freestanding facilities dedicated to this modality, while others are larger, specialized hospital departments. Some treat outpatients exclusively, while others mix inpatients, outpatients, and emergent patients.
The purpose of this article is to identify several key issues that are crucial to successful MRI facility design, regardless of facility size or complexity.
Design strategies
A well-designed facility cannot replace good delivery of medical care or the efficient management of an MRI center; but if the facility is designed creatively, it can enable radiologists and staff to perform their jobs to the best of their abilities.
Similarly, a soothing, healing environment helps comfort fearful patients and reduces their apprehension of the unknown, ultimately resulting in greater patient compliance. Such an environment also can help lower staff stress levels, leading to greater productivity and work satisfaction.
For many people, a building’s image reflects the quality of care provided within. Considering that patients may be apprehensive of the MRI scanner itself, various approaches to incorporating medical equipment into room design can be employed to reduce patients’ anxiety. A room that provides "positive distractions" will help take a patient’s mind off immediate medical concerns. Reduced patient stress leads to improved workflow and greater operational efficiency.
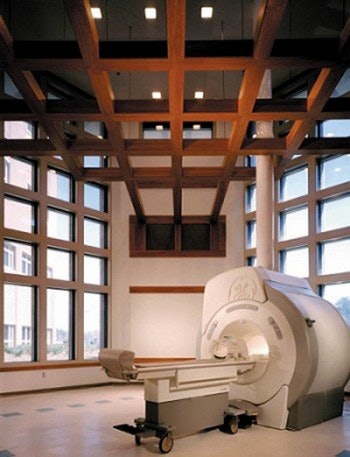 |
| The MRI suite at the Womack Army Medical Center at Fort Bragg, NC, incorporates a floating ceiling grid, natural day lighting, and a view of the outdoors. These "positive distractions" help reduce patient anxiety and apprehension. Architect: SmithGroup; photo: Justin Maconochie/Hedrich Blessing. |
Workflow
Design begins with workflow. The highly repetitive patterns of movement for staff and patients between different activity areas determine optimal facility layout. Various internal traffic patterns need to be considered for patients, technologists, radiologists, nurses, and support staff, while also considering the flow of materials, supplies, images, and information.
Equipment installation routes are critical. Often the scan room is located at ground level along the building’s perimeter. A removable access panel facilitates installation and/or replacement of the magnet.
But magnets need not be limited to ground-floor perimeter locations. When above ground or internal to the building, clearances and structural capacity below the scan room -- and along the entire installation route -- must be sized to accommodate the magnet’s weight, which can be considerable. Some magnets are extremely susceptible to vibration, and most are affected by large, moving metal objects such as elevators and motor vehicles .traveling nearby.
Staff workflow differs significantly from patient flow. For example, the control technologists spend most of their time in or near the control room, the scan room, and the computer room. Radiologists require frequent access into and out of the control and scan rooms (ideally without having to pass through patient waiting areas), especially if the magnet is used for interventional procedures.
In contrast, patients are intentionally kept away from these areas unless first screened and accompanied by authorized and trained personnel. The American College of Radiology recently devised MRI safety guidelines that divide the MRI suite into four discrete "safety zones" to control site access (American Journal of Roentgenology, June 2002, 178:6, pp.1335-1353).
Keep in mind that security requirements prohibiting patient access into procedure areas may conflict with life safety requirements assuring prompt emergency egress from any area within the suite. Often agencies issuing building permits need to be educated regarding MRI security needs, and security devices such as locks and card keys must permit emergency evacuation from an area to which they are restricting access.
In addition to simplifying workflow, the suite should be planned in such a way that the magnet’s 5-gauss line (exclusion zone) is contained vertically and horizontally entirely within the scan room. In some instances this may require supplemental magnetic shielding, which in turn can add significant weight and the need for increased structural capacity. If the 5-gauss line extends beyond the exam room, it must extend only into restricted areas with visual notification of this condition.
Acoustics
The MRI examination is an inherently noisy procedure. A variety of audio and video systems are available to mask ambient noise and distract patients. Although most noise originates in the magnet’s bore, acoustic damping of walls, floor, and ceiling may provide an extra measure of comfort. For example, consider placing fabric-wrapped acoustic panels with a high noise reduction coefficient (NRC) on the walls and ceiling. An acoustic consultant experienced in MRI room design can assist with acoustic design issues.
Lighting
Two lighting levels should be provided in the MRI scan room: A low level of ambient lighting is suggested in the area around the magnet’s bore and the patient couch. (A higher-intensity focused light may supplement the low ambient light level around the couch, especially for interventional procedures.) A higher lighting level should be provided around the magnet’s perimeter for servicing and routine maintenance.
Direct lighting that shines into the patient’s eyes should be avoided. Fluorescent lamps and certain types of electronic dimmers may be contraindicated because they create radiofrequency (RF) disruption and may degrade image quality. Incandescent lamps with a special reinforced tungsten filament are recommended, as the magnetic field will quickly destroy standard lamp filaments. Direct-current (DC) lighting works better in an MR environment than does alternating current (AC).
The control room should also have two lighting levels that are equal to the scan room’s levels. Balancing the light levels in both rooms reduces glare along the control room window.
Technical considerations
Specific requirements may vary among magnet types. Here are some general considerations for an MR facility (The Architecture of Imaging, AHA Press, Chicago, 1995, pp. 271-273).
Functional requirements
- A hand-washing sink is recommended in all patient exam rooms. However, plumbing lines should be routed so as not to disrupt the continuous RF shielding. Often the sink is located outside of the MR scan room to accomplish this.
- Patient dressing, prep, lockers, and toilets should be provided in close proximity to the scan room. Adult and pediatric holding areas with medical supervision and lockable storage for medication should be provided just outside of the scan room (coordinate with ACR MR safety recommendations.)
- The control console should be configured for direct view of the patient’s head.
- Consider a dedicated reading area near the scan room.
- Adequate equipment/supply storage in the scan room and clean and soiled utility rooms nearby will minimize staff travel time.
- Nonferrous oxygen, suction, etc. services should be available in the scan room. Often, permanent gas systems are preferred over portable units as they reduce the risk of having ferrous containers carried into the MR environment in response to an emergency. Also, special nonferrous equipment (gurneys, crash carts, IV poles) must be considered (coordinate with ACR MR safety recommendations).
Human factors
- Consider providing a room or alcove for patient education prior to the MR exam.
- Every effort should be made to relieve patients’ anxiety, with comforts such as natural indirect day lighting and sound control, and basic functional elements such as coherent directional signs and corridor circulation.
Technical issues
- Special structural support for floor-, wall- and ceiling-mounted equipment should be provided in accordance with approved structural calculations and details.
- Adequate access routes and structural capacity should be provided for installation, maintenance, and/or replacement of large equipment.
- Removable access panels should be provided in ceiling, roof, or walls to enable equipment installation and replacement.
- An oxygen-monitoring system should be provided for superconducting magnets.
- Locate the computer equipment room adjacent to scan room(s) for direct connection via a penetration panel.
- Provide additional power and air-handling capacity for future equipment upgrade/replacement.
- Adequate ceiling height must be provided in the scan room and throughout installation access routes.
- Adequate space must be provided for dedicated chillers, or other types of cooling equipment. These are not typically provided by the vendor, and are not often indicated on vendor drawings, thus they are sometimes overlooked.
- Adequate cryogen venting must be provided for superconducting magnets.
- Wave guides or filters must be installed where the RF enclosure is penetrated. Consult the shielding vendor during design as necessary.
- Substantial ferromagnetic objects must be avoided within certain distances of the magnet’s isocenter. Ferromagnetic reinforcement and major steel beams in the floor and ceiling may need to be limited to avoid unshimmable inhomogeneities.
- Consideration needs to be given to the location of other nearby imaging devices, such as other magnets, gamma cameras, and CRTs, as well as motors, elevators, electrical transformers, moving steel equipment or vehicles, and mechanical equipment rooms as they may affect, or be affected by, the magnet’s field.
- Introduction of metal objects or unauthorized traffic and personnel must be prohibited into restricted zones of the MR facility.
AuntMinnie.com contributing writer
July 22, 2002
Bill Rostenberg is a vice president in the San Francisco office of SmithGroup, Inc. Architects and Planners (www.smithgroup.com). He is the author of The Architecture of Imaging and Facility Design for Medical Imaging Workstations. Rostenberg is a fellow of the American College of Healthcare Architects and the American Institute of Architects. He is a guest instructor on health facility design at the Harvard University Graduate School of Design, professional development program, in Cambridge, MA. Rostenberg can be contacted at 415-365-3463 or at [email protected].
Related Reading
Finding the right space for a new imaging center, July 15, 2002
The Architecture of Imaging, January 31, 2002
Baltimore VA survey says human factors count in soft-copy reading, August 29, 2000
Strategic planning key to PACS installations at imaging centers, August 21, 2000
Copyright © 2002 AuntMinnie.com