Accurate assessment of the lymphatic system has proved to be an elusive pursuit, with rather mysterious origins. More than 200 years ago, the Scottish anatomist and teacher Dr. William Hunter was the first to map the lymphatic system comprehensively in his Medical Commentaries (1762-1764). That much seems clear.
But was it Hunter -- or his one-time student and later adversary Dr. Alexander Munro, secundus -- who conceived the notion that the lymphatic system is absorbent, and distinct from circulation? And in any case, hadn't their predecessor, Dr. Friedrich Hoffman, set the stage for them both with his concept of the body as a hydraulic machine? (Medicina rationalis systematica, 1730).
These discoveries, whoever made them, would lead to new answers and further mysteries surrounding the function of the lymphatic system. Today's doctors have a wealth of knowledge at their disposal, but still lack a safe and reliable method of evaluating the labyrinth of lymphatic vessels, nodes, and organs that cleanse the blood, and play a central role in immune system function.
There are excellent reasons to keep searching. Adequate visualization of the lymph nodes is crucial for evaluating benign disease, as well as primary tumors and metastases in the lymph nodes and nearby organs. Until very recently, however, lymphography has generally been limited to finding lymph nodes, and sometimes detecting their enlargement or inflammation.
From the 1930s until the 1990s, the only imaging method available was x-ray lymphography using oil-based contrast agents. The difficulty and invasiveness of this fluoroscopic procedure, however, combined with a risk of embolization of the pulmonary capillary vessels, led to a search for alternative solutions. The development of new contrast agents in the past decade has opened the door to visualization of lymph node pathology as well as morphology.
The quest for a better agent continues. One CT imaging technique detects lesions using an iodinated nanoparticle-based medium originally developed for MR of the liver. Lymphoscintigraphy with the aid of sulfur and human serum-based radiocolloid agents has also been successful, though enhancement has generally been limited to the superficial lymphatic system. FDG-PET does a good job of visualizing the larger lymph node tumors and assessing treatment response, while research in targeted radionuclides offers great potential for the future.
These days, MR lymphography might just be the hottest ticket. It is currently being investigated with a variety of contrast agents, including iodinated and gadolinium-based media, superparamagnetic iron oxide particles (SPIO), and, more recently, ultrasmall superparamagnetic iron oxide particles (USPIO) as MR markers. The diminutive size of USPIO particles facilitates their absorption into the lymph nodes rather than the liver, where particles larger than 50 microns tend to migrate.
Following administration of a USPIO agent, either intravenously or interstitially, the tiny iron particles begin to accumulate in the macrophages of normal lymph nodes. The accumulated particles reduce the signal intensity of normally functioning nodal tissue by enhancing spin dephasing and shortening relaxation time in T2-weighted MRI. Malignant tissue, which does not absorb the superparamagnetic particles, tends to be hyperintense in comparison.
At the 2002 European Congress of Radiology in Vienna, three investigators presented the results of MR lymphography studies using Sinerem, (Guerbet, Aulnay-sous-Bois, France). Sinerem is the trade name in Western Europe and Brazil for ferumoxtran (Combidex, Advanced Magnetics, Cambridge, MA) an investigative dextran-coated USPIO agent developed specifically for MR lymphography.
In studies to date, the agent's performance has been adequate, but with significant limitations. So it remains to be seen whether Combidex/Sinerem -- or any other USPIO-enhanced compound -- will prove to be sensitive enough to aid significantly in the diagnosis of lymph node pathology.
In another ECR presentation, Dr. Christoph Herborn from University Hospital in Essen, Germany, discussed an alternative approach: MR lymphography in rabbits following interstitial injection of an albumin-binding gadolinium chelate known as MS-325 (Epix Medical, Cambridge, MA).
The two agents are of course quite different, not only in design but in stage of development. While Sinerem is thought to be nearing regulatory approval for multiple uses, MS-325 isn't as far along in the process. And MS-325 is currently being used in phase III clinical trials for MR angiography of the peripheral vessels, not lymphography.
Still, initial lymphography results in animals have been impressive. MS-325 reversibly binds to albumin, the most common protein in the blood, which enables it to pass easily into the cellular membrane of lymph nodes. And like USPIO-enhanced agents, the compounds are absorbed into normal lymph node tissue but not malignancies, enabling researchers to distinguish between the two.
Herborn described the mechanisms that enable MS-325 to image the lymph system using MRI.
"Following injection into the vascular system, the (MS-325) molecule is bound to albumin, and following this binding, the molecular rotation rate is significantly decreased while the relaxivity increases approximately eightfold," he said. "Since it is well known that there is a considerable amount of albumin in the lymphatic tissue, our hypothesis was that MR lymphography (using MS-325) would be helpful for the assessment of tumor invasion into lymph nodes."
Albumin's binding properties enable exogenous contrast agents such as MS-325 to remain in the blood longer, Herborn said. The protein has previously been used in certain nuclear medicine applications, such as in gallium-67 for scintigraphy.
Herborn's group performed MRI both before and after injection of the tumor-bearing agent, enabling the evaluation of both normal and tumor-bearing nodes. After the animals were euthanized, the researchers were able to correlate the results of MR lymphography with histopathology.
Along with colleagues Dr. Stefan Ruehm, Dr. Thomas Lauenstein, Dr. Florian Vogt, and Dr. Jörg Debatin, Herborn evaluated the performance of MS-325 in six white New Zealand rabbits. The animals were completely anesthetized, then injected subcutaneously in both dorsal footpads with 0.5 ml (each side) of the undiluted MS-325 agent.
Imaging was performed on a 1.5-tesla scanner (Magnetom Sonata, Siemens Medical Solutions, Erlangen, Germany) equipped with high-performance gradients. Imaging consisted of a 2-D axial localizer acquisition (TrueFISP) followed by a 3-D VIBE sequence. "VIBE is a unique sequence offering significant fat-suppression characteristics, which benefit MR lymphography in general," Herborn said.
After the first round of imaging, the animals were injected with VX-2 tumor cells in the left flank, and later reimaged about three weeks later using the same sequence.
"The VX-2 tumor is a squamous cell epithelial testicular carcinoma that frequently metastasizes, and is well-established for the induction of metastases in animal research," Herborn said. The imaging protocol was repeated at 5, 10, and 15 minutes following contrast administration. All of the animals were euthanized within 24 hours of the second imaging sequence.
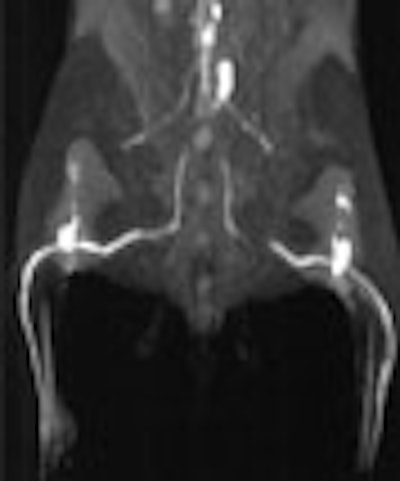
The injection of MS-325 enabled clear delineation of four consecutive lymph node groups, including the distal and proximal popliteal lymph nodes, inguinal, and common iliac/paraortic lymph nodes, Herborn said.
The brightest enhancement was achieved in the popliteal lymph nodes and associated draining vessels. Peak enhancement in these nodes occurred approximately 5 to 15 minutes following administration of the compound, Herborn said. The more proximal iliac and paraaortic lymph nodes achieved peak enhancement in about 30 minutes.
"The tumor invasion was visible as a signal void within the lymph nodes in the side ipsilateral to the VX-2 tumor," Herborn said. "These imaging findings were pretty well seen on the oblique views as well as the coronal views, and some of the structures like the thoracic duct could (also) be assessed." Even subtle tumor invasions, involving less than 25% of the node, could be visualized by rotating and postprocessing the images, he said.
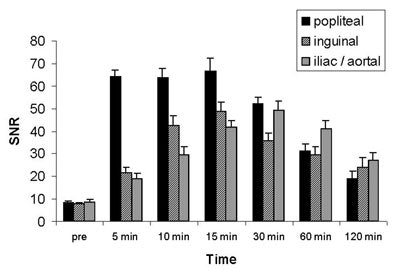 |
| Above, bar graphs represent time course of tumor-invaded lymph node area compared to normal lymphatic tissue. While enhancement of unaffected tissue was similar to healthy lymphatic tissue, significantly decreased signal was observed within metastases. Error bars represent mean standard errors. SNR = signal-to-noise ratio. |
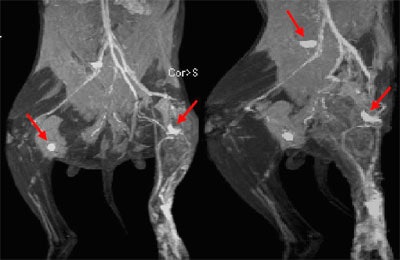 |
| Above, coronal maximum intensity projection (MIP) image of interstitial MR lymphography in two rabbits with an implanted VX-2 tumor in left hindleg. Tumor invasion of left proximal popliteal lymph node can be assessed as circumscribed signal loss of tumor-bearing part (arrows) ipsilateral to the tumor in both animals, whereas contralateral nodes show homogeneous and bright enhancement. Note tumor invasion in enlarged iliac lymph node of the rabbit shown at right. Images and graphics courtesy of Dr. Christoph Herborn. |
"The correlation between MR lymphography and histopathology was excellent," Herborn said. "There was 100% agreement for the examination of normal and tumor-invaded lymph nodes, leading to a sensitivity and specificity of 100%. Interstitial injection of MS-325 permits the differentiation of normal and tumor-bearing lymph nodes, which warrants further examination in humans."
Smaller nodes difficult to see with USPIO-enhanced Sinerem MR
Another ECR presenter discussed the ability of USPIO-enhanced ferumoxtran (Sinerem) to diagnose lymph node metastases. Dr. Giovanni Morana and colleagues from the University of Verona in Italy examined 9 patients with suspected axillary lymph node metastasis from breast carcinoma.
Following intravenous administration of the agent, the patients underwent 3 MR imaging sequences on a 1.5-tesla machine using a surface coil, including spin-echo T1-weighted; TURBO spin-echo diffusion/perfusion-weighted, and FLASH T2-weighted sequences. Images were acquired and diagnosis made both pre-and postcontrast, based on subjective criteria of shape and size. All patients were evaluated surgically within 15 days of imaging, and the results sent for pathological examination.
In all, 110 lymph nodes were identified at surgery, 69 of which were visible on MRI. MRI missed five metastatic lymph nodes, Morana said. Overall specificity, sensitivity, and positive and negative predictive values of MRI with Sinerem were 28.6%, 97.7%, 80%, and 81.1% respectively. The mean diameter of lymph nodes not visible on MRI was 2.5 mm.
The signal intensity was highest in the true-positive cases, but was also high in the false-positive cases, Morana said. "One problem is that we were not able to recognize inflammatory lymph nodes, as they were hyperintense on the T2 sequences... Also, fat infiltration can give a homogeneous appearance of the lymph node, so it is very important in our series to utilize the fat-saturation sequences." When visible, metastatic involvement was often characterized by a basket-like ring of hyperintensity surrounding the positive node.
"MRI using Sinerem contrast has a low sensitivity for defining small lymph nodes, but when lymph nodes are visible, the technique has high sensitivity for detecting metastases," Morana concluded. "When the objective data are combined with the subjective impression of the radiologist, the results are quite satisfactory."
Sinerem MR detects most, but not all, rectal lymph node metastases
Another study looked at the ability of MR lymphography with Sinerem to detect metastatic lymph node involvement in primary rectal cancer.
Dr. Wassilios Pegios from the University of Frankfurt, Germany, and colleagues imaged 8 rectal cancer patients with Sinerem-enhanced MR lymphography, in a preoperative evaluation of lymph node metastases.
MR images were acquired both before, and 24-36 hours after, intravenous administration of 2.6 mg of ferumoxtran (Sinerem) per kg of body weight, Pegios said. For each patient the investigators acquired T1- and T2-weighted spin-echo sequences, as well as T2-weighted gradient-echo sequences, using a Helmholtz coil.
Histopathology was correlated with MRI in all patients post-surgery. Lymph node pre-and postcontrast images were evaluated subjectively for signal intensity and rated as increased, decreased or no change following contrast administration, and also rated as homogeneous or heterogeneous.
A total of 108 lymph nodes were evaluated histopathologically, and the results correlated with MRI. MRI detected 6 of 7 pathologically proven metastases, but missed a 6 mm metastasis. The metastatic lymph nodes detected by MR were 6-10 mm in diameter (n=3), 16-20 mm (n=2), and a single 25 mm node.
Overall, the metastasized lymph nodes had a heterogeneous signal intensity on MRI, with contrast uptake in normal tissue, and malignant regions characterized by a signal void. Benign nodes were more homogeneous in appearance. However, MRI was not able to visualize all of the lymph nodes found at pathology, even one as large as 16 mm. A rectal coil would be needed to adequately evaluate the rectal lymph nodes, Pegios said.
"MR lymphography with employment of new iron oxide contrast materials is a promising imaging modality for the detection of lymph node metastases, but with many limitations," he concluded, adding that comparisons with other studies are complicated by widely varying imaging techniques and evaluation criteria. A larger study population is needed to further evaluate the potential of this technique, Pegios said.
Poor contrast enhancement in very enlarged nodesFinally, Dr. G. Michna from the University Clinic in Freiburg, Germany presented a study of MR lymphography using Sinerem for the nodal staging of 10 patients who had histologically proven but untreated primary lymphoma. Michna and colleagues measured the signal intensities of 23 lymph nodes ranging from 13 mm to 105 mm in size, both pre- and postcontrast injection.
Comparing the delta of mean values pre- and postcontrast signal intensities in T1- and T2-weighted MR images, the researchers found no significant change in signal intensities. The results suggest that in very enlarged lymph nodes, no active RES cells remain to phagocytise the iron particles due to malignancy, Michna concluded.
Multicenter MR Sinerem trial shows high specificity, flat sensitivity
In May of this year, the results of the first multicenter trial using Sinerem were published in European Radiology.
Dr. Robert Sigal from the Institut Goustave Roussy in Villejuif, France, led a multicenter trial that examined 81 patients with untreated head and neck squamous-cell carcinoma. MRI, both without contrast and with Sinerem, was used to diagnose lymph node metastases no more than 15 days prior to surgery (Eur. Radiol., May 2002, Vol. 12:5, pp. 1104-1113).
Compared with histology, Sinerem MR showed sensitivity and specificity of 88% and 77% for the diagnosis of lymph node metastases. Some false-positive results were due to inflammatory nodes, while false-negative results were due to undetected micrometastases, the authors wrote. Sinerem MR had a negative predictive value of 90%, and a positive predictive value of 51% for the diagnosis of lymph node metastases.
While the specificity and positive predictive value of Sinerem MR were higher than MR without contrast, noncontrast MR showed an unexpectedly high sensitivity and negative predictive value, which did not increase with the addition of Sinerem to the protocol.
Sinerem MR is promising, but remains limited by technical problems, including motion and susceptibility artifacts and spatial resolution, the group concluded.
Advanced Magnetics received an approvable letter from the FDA in June 2000, and is working with the agency to resolve outstanding issues in its bid to market Combidex in the U.S. Since December 1999, Guerbet has been working with the European Medicines Evaluations Agency in an effort to market Sinerem in Europe.
By Eric BarnesAuntMinnie.com staff writer
August 9, 2002
Related Reading
Epix net loss widens, delays MS-325 NDA, July 26, 2002
PET better than CT for lymph node staging in patients with cervical cancer, September 5, 2001
Collapse in proposed merger of Cytogen, Advanced Magnetics, August 28, 2000
Advanced Magnetics agent gets approvable letter, June 22, 2000
Advanced Magnetics reports lower first-quarter results, January 24, 2000
Copyright © 2002 AuntMinnie.com


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)





.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)











