The nascent field of intraoperative MRI has seen a number of technology trends: C-shaped magnets, stand-up magnets, double-doughnut magnets, ultrashort-bore magnets. But all share a common theme -- patients are moved into and out of a stationary magnet for imaging studies.
A Canadian firm may be the first to change this practice with a new dedicated intraoperative MRI scanner that moves to the patient rather than having the patient move to it. IMRIS of Winnipeg, Manitoba, believes that its Neuro II scanner can be a safer and more efficient alternative than intraoperative MRI using a stationary scanner.
For example, often a neurosurgeon needs to capture an up-to-date view of the cranial operative field, which means moving the patient from a surgical suite on an upper floor to an MRI imaging suite on the ground floor. This is time-consuming, and it can be dangerous to move a patient under general anesthesia through an unsterile environment.
Instead, in a suite equipped with a Neuro II scanner, the system comes out of a wall compartment and moves over the patient, the patient is imaged, and the scanner moves back into the compartment. Surgery continues using intraoperative images.

Neuro II is a 1.5-tesla scanner that is suspended from a ceiling using a series of supports that are tied into columns of a building and thus into the building's piers, according to IMRIS president David Graves. Testing on the system indicates that the design is vibration-free and is more stable than a floor-mounted system, he said.
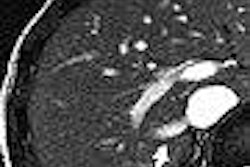
Although the system was conceived by a Winnipeg neurosurgeon, Dr. Garnette Sutherland, it is not limited to craniotomy use, Graves said. "The table is cantilevered so the base of the table is at the foot, so even patients' feet can be in the bore. It can image any portion of the body. We have a series of new applications for spinal surgery, liver surgery, and other indications."
IMRIS has three scenarios for use with its system. The first is the single operating room with the MR scanner in its parking compartment (called a "dog house" by some), out of which it moves to the operating table.
Imaging is possible out of both sides of the magnet. Thus, the second scenario is a two-operating room arrangement in which the scanner moves from one operating room back into the parking area, which has doors on either end, so that when one set of doors is opened, the other set must be closed. The system automatically closes the doors, evacuates, and cleans the compartment air, then opens the other door and moves the scanner into the other operating room.
"This gives you two fully functional operating rooms that can be used intraoperatively or not," Graves said.
A final scenario would turn the second room into a standard diagnostic room that could be used for routine MRI exams. This would be particularly useful for inpatients who have to be sedated, especially at children's hospitals, Graves said, while providing dual use for an expensive piece of capital equipment.
This would seemingly make the system more practical for smaller institutions, and is the exact setup that Wilkes-Barre General Hospital in Pennsylvania is getting. IMRIS has also just completed an install at Children's Hospital of Boston, while another is in progress at Children's Healthcare of Atlanta at Scottish Rite.
Architectural challenge?
The novel design of the Neuro II system, and the fact that in some cases it could have shared uses, could present some architectural challenges. Both infection control and cryogen venting would need to be accounted for in any Neuro II installation, according to Tobias Gilk and Robert Junk, principals in the Kansas City, MO, firm Jünk Architects. Although Gilk and Junk do not have a formal arrangement with IMRIS, they are familiar with the system.
Lighting fixtures in the OR would have to be MRI-compatible, and there are also potential issues involved with MRI compatibility of surgical equipment that might be inadvertently left in the room, Junk said. When you bring patients to stationary MRI scanners for imaging, it's easier to control the environment through safety practices like having patients pass through a ferro-metallic detector.
"I don't want to throw cold water on this, (because) I think this is the wave of the future," Gilk said. "This type of intraoperative imaging is something that is going to be very valuable, but my goal is to make sure people have thought this through."
Graves said the system has been designed to accommodate such concerns. A venting pipe is included in the design to deal with quench events, and IMRIS videos show dotted lines painted on the floor indicating where the magnetic field begins to attract ferrous objects -- one set of lines around where it is parked inside its bay, and another set of lines showing the magnetic field when the magnet is in place over the patient.
The IMRIS technology was developed at Canada's National Research Council Institute for Biodiagnostics (NRC-IBD) by a group of surgeons and scientists headed by Sutherland and John Saunders, Ph.D., an MR scientist at Foothills Hospital Seaman Family MR Research Centre in Calgary, Alberta. A demonstration system is installed there and is used routinely as an adjunct to brain surgery.
IMRIS was formed in 1999, and is funded through venture capital only. Its major OEM partner is Malvern, PA-based Siemens Medical Solutions.
Neuro II has Food and Drug Administration 510(k) clearance, as well Health Canada clearance and the CE Mark for European sales. The company will show its system at the October Congress of Neurological Surgeons (CNS) in Boston, where the firm will stage a full operating room. IMRIS will also be at this year's November RSNA show in Chicago, probably in the Siemens booth.
By Robert Bruce
AuntMinnie.com contributing writer
August 12, 2005
Related Reading
Interventional MRI: Out of the scanning suite and into the OR, July 8, 2005
Construction planning outside the MRI suite, June 9, 2005
Part II: Answers to the 10 questions to ask your architect about MRI suite design, April 7, 2005
Part I: 10 questions to ask your architect about MRI suite design, April 5, 2005
HIPAA compliance strategies for MR control rooms, October 26, 2004
Copyright © 2005 AuntMinnie.com