As Hurricanes Katrina and Rita pummeled the Gulf Coast with a wicked one-two punch, New Orleans was turned into a soggy ghost town, and coastal communities east and west of the crescent city were all but wiped off the map. Beyond the mass media's 24-hour news coverage of the physical and human toll the storms inflicted, stories of individual healthcare providers, imaging centers, and hospital radiology departments didn't receive much attention.
But those of us far away from "hurricane alley" shouldn't lull ourselves into a false sense of security. While the images and stories are fresh in our minds, we should leverage that palpable fear and explore what natural and man-made threats exist for each of us in our own locations.
The hurricanes, because of their scale and ferocity, combined a number of threats to radiology operations. The winds and tidal surges caused structural damage to many buildings. The rains, tides, and failing levies compounded structural damage with profound flooding. And the systemic damage to infrastructure denied electricity, potable water, communications, and natural gas to large areas. The stories coming from the assessment and reconstruction of the Gulf Coast are beginning to show us preparations that were successful in protecting equipment and facilities, as well as those that weren't.
One imaging service provider with multiple locations in the New Orleans area had a very well thought-out emergency plan. It started at the beginning of hurricane season when they insisted on having all of their magnets topped off with cryogen, despite the fact that they weren't scheduled for a fill. Even though protracted electrical outages can cause magnet systems to spontaneously quench as the cryogen slowly warms to the boiling point, that didn't happen at several of this provider's facilities. Despite significant storm and flooding damage, three of four superconducting magnets survived extended power outages without quenching because of the proactive fill, which extended the time before the system would quench.
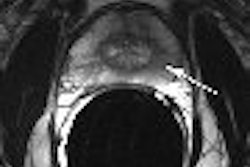
Other facilities, fearing extensive damage to their MRI systems, manually initiated pre-emptive quenches. Under the best circumstances, a quench subjects a magnet to a 500º F thermal shock, which can cause major structural damage. Under other circumstances, a quench can breach the quench tube and cause significant damage to the magnet room and jeopardize the safety of those in the vicinity. It was rumored at one facility that elected to preemptively quench its magnets that the quench tube failed and the pressure from the expanding cryogen blew out the control room radiofrequency window!
Beyond MRIs, all major imaging modalities rely on sophisticated electronics and computer processing. Though cryogens aren't an issue for a CT, water in the sensitive electronics is. Facilities successfully protected the electronic components from water damage by protecting them both from above and below. To keep leaking roofs from dousing electronics, some facilities covered gantries and equipment with sturdy plastic, taped in place. To keep processors and gradient cabinets from becoming swamped in a flood situation, everything that could be lifted up off the ground was moved as far off of the floor as possible.
Many hospitals and imaging facilities had emergency generators to help restore power, but too many of these sites had generators or other critical supplies in basements or other low-lying areas that were flooded.
The cascade of failures and the glimmers of success from Hurricanes Katrina and Rita are examples to each of us that emergency preparedness can pay tremendous dividends. Even for those of us who aren't in the likely path of Gulf hurricanes, we may have to contend with earthquakes, tornadoes, fires, ice, snowstorms, or even man-made blackouts such as the one that gripped much of the northeastern U.S. in 2004.
So each care provider, hospital, and imaging facility should assess its emergency preparations and forecast its own emergency response. Below are a number of considerations that should serve as a starting point for conversations about a plan for emergency preparedness at a facility.
- What are the likely/possible natural disasters to affect the area?
- What are the likely/possible man-made disasters to affect the area?
- Would electrical power be interrupted?
- Would other utilities (natural gas, telecommunications, etc.) be interrupted?
- What equipment would be inoperative during the outage?
- What equipment could be damaged by the outage?
- What equipment should be provided with critical or backup power?
- If the utility service is not quickly restored, what other risks are there?
- Would patients and staff be able to get to the facility?
- Would patients or staff be trapped at the facility?
- How critical is each patient care service provided at the facility?
- In order of importance, how does the facility protect the equipment needed to support each service?
- If the facility does not have the resources on site, who can provide them?
At some point, each of us will likely face some extraordinary condition and have to work through it. If our jobs were manufacturing hubcaps, for example, a few days or even a few weeks out of commission would certainly be a personal burden. But for those of us charged with providing critical components of healthcare to our communities, minimizing interruptions and returning to service has a far greater urgency.
By Robert Junk and Tobias Gilk
AuntMinnie.com contributing writers
December 26, 2005
Reprinted from www.mri-planning.com by permission of the authors. If you would like more information on any aspect of MR facility design or safety, please contact Robert Junk or Tobias Gilk at Jünk Architects.
Related Reading
MRI vendor suite templates: What they don't show, December 8, 2005
Hitting the ceiling over HIPAA-required walls, December 6, 2005
Burying MRI construction mistakes: What you cannot see affects what you can, November 23, 2005
The new 'MR Safe': Language changes for the FDA, October 27, 2005
Cost of MRI mishaps makes safety investment profitable, October 14, 2005
Copyright © 2005 Jünk Architects, PC