WASHINGTON, DC - MRI should be the first imaging test, rather than ultrasound, for pregnant women suspected of having appendicitis, according to a study presented at last week's American Roentgen Ray Society (ARRS) meeting.
Researchers from the Warren Alpert Medical School at Brown University in Providence, RI, found that MRI visualized the appendix in 80% of cases, compared with only 7% for ultrasound, and achieved 100% sensitivity and specificity. Lead study author is Dr. David Grand, a radiologist and an assistant professor of diagnostic imaging at the school.
"We determined that MRI is the test of choice," study co-author Dr. Joseph Konrad, a diagnostic imaging resident, said during his ARRS presentation. "It is safe and extremely accurate. When performing an ultrasound prior to an MRI, [ultrasound] adds little diagnostic yield."
Contributing to fetal loss
Appendicitis during pregnancy is fairly common, as the condition is seen in approximately one in every 1,500 pregnancies, according to the authors. Appendicitis is also the top nonobstetrical reason for emergent surgery.
"Early detection of appendicitis is imperative, because perforation can lead to fetal loss in up to 20% of the time," Konrad added. "With an early understanding of appendicitis, we can decrease fetal loss to approximately 1.5% of the time, if appropriate therapy is undertaken."
Currently, CT is the primary modality for evaluating appendicitis in adults. Ultrasound is reportedly useful, Konrad noted, but the modality is limited in identifying appendicitis in pregnant women and obese adults, partly due to the location of the appendix. The use of MRI, meanwhile, currently is gaining popularity because of its efficacy in identifying the appendix and its lack of ionizing radiation.
At Rhode Island Hospital in Providence, the current protocol is for pregnant patients with suspected appendicitis to initially undergo an ultrasound exam. The first goal is to determine if the appendix is normal.
"If we can't identify the appendix, we look for additional pathology or other etiologies the patients may have," Konrad said. "Specifically, we are looking for ovarian pathology."
If physicians can't identify the cause or source of the pain, the patient proceeds to an MRI exam.
Appendix visualization
The retrospective study analyzed pregnant patients from January 2009 to January 2011 who presented for suspected appendicitis. Researchers reviewed records to determine if the appendix could be seen, the size of the appendix and its appearance, and any signs of appendicitis. If no source of pain was evident, Konrad and colleagues looked for an alternate cause and whether the etiology was discovered by ultrasound, MRI, or both.
The study also investigated whether the imaging results correlated with the surgical pathology.
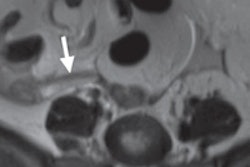
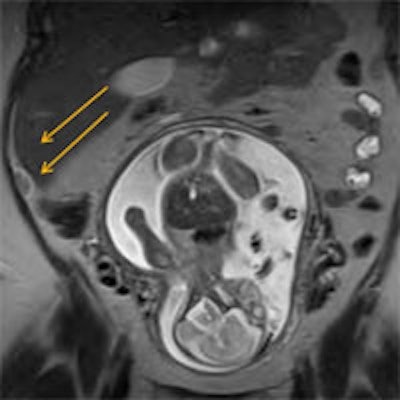
MRI exams were conducted on a 1.5-tesla magnet with a pelvic coil. The imaging protocol included axial, sagittal, and coronal T2-weighted steady-state fast spin-echo (SSFSE) sequences, as well as axial steady-state free precession (SSFP), and axial short-tau inversion-recovery (STIR) sequences. Ultrasound was performed by a certified technologist, with radiologist backup, as needed.
The study included 140 patients, with 115 MRI exams, 117 ultrasound scans, and 91 individuals imaged with both modalities.
Of the 115 women who were imaged with MRI, the appendix could be seen in 92 (80%) of cases, compared with 23 occasions (20%) when the appendix was not visualized. Among the patients whose appendix could not be seen on MRI, 18 women had no etiology of pain and were treated as if they did not have acute appendicitis. The other five patients with pain were found to have ureteral stones, transverse colitis, inguinal hernia, and calyceal ruptures in two cases.
Among the 92 patients whose appendixes were seen, 71 women (77%) were negative for appendicitis, and physicians were able to diagnose an alternative cause of the pain in 10 cases.
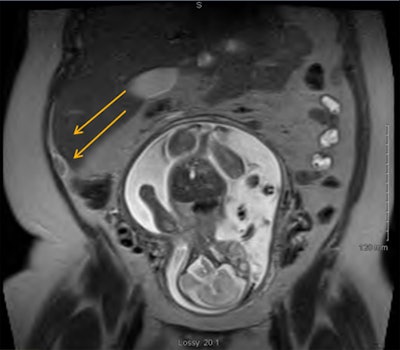
Acute appendicitis was diagnosed in 21 patients (23%), of which 19 cases were proved by pathology. Also, one woman had a neuroendocrine tumor, and one person had mural endometriosis.
A further analysis of the 71 women who were negative for appendicitis found 10 other causes of their pain, including an ovarian cyst, degenerating fibroid, cholecystitis, and calyceal rupture.
MRI also achieved 100% sensitivity and specificity for acute appendicitis in pregnant patients and provided an alternative diagnosis in 14% of cases.
Ultrasound's efficacy
Among the 117 ultrasound scans, the appendix could not be visualized in 109 women (93%). Of these, physicians were able to identify another cause of the pain in three patients (2%), while 84 pregnant women (77%) were sent for an MRI exam
Of the eight appendixes seen on ultrasound, five cases were determined to be normal and three individuals had acute appendicitis. Even when ultrasound cases were ruled normal or acute appendicitis, all of these patients proceeded to MRI.
"We can see that the MRI visualization rate of the appendix is much higher than ultrasound, 80% to 7%," Konrad said. "The most interesting thing is that when the appendix was not visualized on ultrasound or was visualized on ultrasound, many patients still went on to MRI for confirmation."
Konrad cited two limitations of the study: its retrospective approach and real-time imaging by a radiologist was not obtained in all cases.