Fatty liver is an independent risk factor for heart failure in obese patients -- that is, those with a body mass index of 30 or higher, according to a new study published online January 26 in Radiology. The finding suggests that concrete interventions to stave off nonalcoholic fatty liver disease, also called hepatic steatosis, could help these patients stay healthy.
In fact, hepatic steatosis is the most common liver disease, with up to 30% of the general population developing it, according to the researchers from the Netherlands. The rate is even higher -- between 70% and 90% -- for patients who are obese or who have type 2 diabetes. It's considered a manifestation of metabolic syndrome, which is a group of risk factors such as high blood pressure and cholesterol level, as well as excess abdominal fat.
 Dr. Ralph Widya from Leiden University Medical Center.
Dr. Ralph Widya from Leiden University Medical Center.So reducing the risk of fatty liver disease in obese patients through interventions could be key to improving their health, lead author Dr. Ralph Widya from Leiden University Medical Center told AuntMinnie.com via email.
"This independent association between fatty liver disease and heart failure suggests that focusing on preventing liver disease with interventions such as dietary changes could help obese patients," he said.
The epidemiology of obesity
Data for the research came from the Netherlands Epidemiology of Obesity (NEO) study, which was conducted between 2008 and 2012. The NEO study included 6,673 men and women between the ages of 45 and 65 who had a body mass index (BMI) of at least 27.
For this study, Widya and colleagues included 714 men and women who had undergone proton MR spectroscopy to gauge their hepatic triglyceride content -- a measure of fat in the liver -- and cardiac MRI to assess left ventricular diastolic function. Of these 714 patients, 47% were categorized as overweight and 13% were classified as obese (Radiology, January 26, 2016).
Diastolic function is the phase of the heartbeat when the heart relaxes to fill with blood, and abnormalities in this function are a key factor in patients with heart failure, the authors wrote.
Widya and colleagues found that an increase in hepatic triglyceride content was associated with a decrease in mean left ventricular diastolic function in obese patients. Furthermore, this association existed independently of metabolic syndrome, which suggests that for obese people, fatty liver itself could pose a risk of heart disease above and beyond known cardiovascular risk factors that are clustered within metabolic syndrome.
Diastolic function was compromised in the obese subgroup, as demonstrated by a lower E/A ratio (with "E" representing early and "A" representing late ventricular filling velocities), compared with normal-weight and overweight subgroups. In a healthy heart, the early velocity is greater than the late velocity.
| Cardiac function in patients by weight | |||||
| Weight | Median hepatic triglyceride content | Diastolic function (represented by E/A ratio) | |||
| Normal weight (BMI: < 25) | 1.49% | 1.36 | |||
| Overweight (BMI: 25-30) | 3.44% | 1.32 | |||
| Obese (BMI: ≥ 30) | 7.64% | 1.20 | |||
"Our results may be of importance in cardiovascular risk stratification in obesity, because there is a large variation in the degree of hepatic steatosis in obesity," Widya said in a statement released by RSNA.
The bigger picture
How might these findings influence clinical practice? More research needs to be done, but the study results may help radiologists take a wider perspective when they encounter liver disease, Widya said.
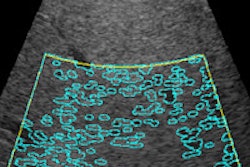
"Just be reminded that when you see a fatty liver in a patient, it may not be straightforward, but rather a symptom of a number of inflammatory pathways that may negatively influence heart function," he said.