
CHICAGO - MRI-based computer-aided detection (CAD) can improve detection sensitivity for prostate cancer for most readers, while reducing reading time fourfold, according to a Tuesday presentation at RSNA 2016.
The study examined the clinical use of a CAD system based on multiparametric MRI of prostate cancer, comparing CAD as a first reader to unaided interpretation of prostate cancers by three readers, recording lesion size, a five-point confidence score for both reading methods, and interpretation time. Use of the CAD system resulted in greater lesion-detection sensitivity for most readers.
"CAD used as the first reader significantly improves the sensitivity in detecting lesions with a diameter of 10 mm or greater and [Gleason] score greater than 6, without altering specificity," said Dr. Valentina Giannini from Candiolo Cancer Institute in Italy.
An accurate tool
Correlation with radical prostatectomy has shown that multiparametric MRI, which associates T2-weighted imaging with diffusion-weighted imaging, dynamic contrast-enhanced imaging, or H1-spectroscopy, has excellent sensitivity for detecting and localizing clinically significant cancers.
 Dr. Valentina Giannini from Candiolo Cancer Institute.
Dr. Valentina Giannini from Candiolo Cancer Institute.Unfortunately, the technique also delivers high interreader variability, and it is time-consuming and labor-intensive, Giannini said. Moreover, depending on the radiologist's experience level, as many as 30% of prostate cancer detections turn out to be false negatives.
An April 2016 study of standalone CAD performance by the group revealed high sensitivities for peripheral zone cancers in the range of 96% per lesion and 97% per patient for the multiparametric imaging-based CAD.
The CAD algorithm relies on "kinetic parameters from dynamic contrast-enhanced MRI, as well as T2-weighted images and [apparent diffusion coefficient (ADC)] maps," Giannini told AuntMinnie.com after her talk. "We use just the intensity for the T2-weighted images, we normalized and corrected the ADC map, and we used some novel parameters from the dynamic contrast-enhanced images because we didn't use k-trans," she said. K-trans is a more common parameter for this type of algorithm, but the group found that it works against accuracy.
Assessing performance
Although the standalone results have been quite promising, "the impact of CAD on radiologists' performance ... was never assessed," Giannini said in her presentation.
This study brought the CAD into clinical use, comparing the sensitivity and specificity of three expert readers for detecting prostate cancers, both unassisted by CAD and with CAD used as the first reader. The researchers also assessed whether using CAD as the first reader could reduce reporting time and interobserver variability.
The readers first reported CAD in the first-reader paradigm, by analyzing the probability map of the CAD results superimposed on the T2-weighted MR images, and confirming the CAD marks that they considered to be prostate cancers.
Six weeks later, they reviewed the cases in random order without the use of CAD, scrolling through all MR images including T2-weighted, diffusion-weighted, and dynamic contrast-enhanced images. They used the Prostate Imaging Reporting and Data System (PI-RADS) for the unassisted reads and a five-point confidence score for all findings, recording interpretation time for both methods. They reported per-patient and per-lesion sensitivity and specificity, comparing them using the McNemar test. Finally, Fleiss' kappa statistics were used to assess interobserver agreement.
The dataset consisted of 35 patients who had at least one clinically significant tumor (38 prostate cancers) and 54 negative patients who remained so during a one-year follow-up.
The mean per-patient sensitivity of first-reader CAD and unassisted reading did not differ significantly (81% versus 88%, p = 0.105) when looking at lesions of all sizes and Gleason score levels.
"Considering all the lesions, we observed an increase in sensitivity for all readers when using the CAD system," Giannini said. "However, it was interesting that when we stratified tumors above Gleason score 6, we observed a significant increase in sensitivity. ... Similarly, stratifying tumors for maximum diameter of 10 mm or larger versus 6 mm or larger also increased the sensitivity."
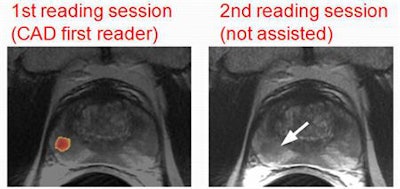 Three expert observers read each image twice, first with the aid of CAD and again six weeks later, unassisted and randomly ordered. Images courtesy of Dr. Valentina Giannini.
Three expert observers read each image twice, first with the aid of CAD and again six weeks later, unassisted and randomly ordered. Images courtesy of Dr. Valentina Giannini.CAD sensitivity rose significantly -- from 81% to 91% -- for patients who had a Gleason score of 6 or greater and a lesion size of 10 mm or larger.
Even so, the increase in specificity was not significant (75.3% versus 78.4%, p = 0.25) when using first-reader CAD. The average reading time fell sharply with the use of CAD, from an average of 220 seconds to an average of 60 seconds (p < 0.0001). Finally, a Fleiss' kappa analysis of interreader agreement increased with CAD, both per patient (0.55 versus 0.60) and per lesion (0.46 versus 0.55).
As for study limitations, "we used the first-reader paradigm for CAD, which is quite unnatural for this type of tumor," Giannini said. "We need to test other reading paradigms." The next study will also be a multicenter trial.
This type of CAD may be an attractive reading strategy to work into the clinical environment, especially if multiparametric MRI results are used to select patients for biopsy, she concluded.




















