By taking MRI measurements of the brain's functional network connectivity within two weeks after a patient experiences cardiac arrest, clinicians may be better able to predict their clinical outcomes, according to a study published online on October 18 in Radiology.
Researchers from the U.S. and Europe are hopeful that the degree of connectivity between brain networks could become a novel prognostic biomarker that could help clinicians make treatment decisions for these severely injured patients and allow families time to prepare for potentially less than favorable outcomes (Radiology, October 18, 2017).
"We recommend obtaining a brain MRI in all patients who have neurological or cognitive impairment following cardiac arrest," said lead author Dr. Robert Stevens from Johns Hopkins University. "This is game-changing information about what happens in the brains of people who suffer cardiac arrest."
Personal connection
Cardiac arrest strikes approximately 535,000 people in the U.S. annually, according to the American Heart Association. For patients who do survive, their outcomes vary from full recovery to long-term functional disability and cognitive impairment.
For more severe cases, "current prognostic models fail to predict coma emergence and cognitive recovery with a degree of accuracy and reproducibility that would be useful at single-subject level," the authors wrote.
 Dr. Robert Stevens from Johns Hopkins University.
Dr. Robert Stevens from Johns Hopkins University.Stevens and colleagues have had an ongoing interest in the use of advanced MRI protocols and quantitative brain mapping to identify brain injuries related to cardiac arrest and to help predict how patients will recover. For Stevens, the research is also personal.
"My own father suffered a cardiac arrest and, although his doctors were very pessimistic, he was able to achieve an excellent recovery," he wrote in an email to AuntMinnie.com. "Conversely, another member of my family had hypoxic-ischemic injury at birth and never recovered. Again, there was a lot of equivocation regarding his potential outcomes. These experiences led me to believe that we need to find better ways to classify and care for these patients."
The researchers retrospectively identified subjects from a prospective cohort of patients who were admitted with severe brain injury to the intensive care units at two hospitals in France and one medical center in Belgium between July 2007 and October 2013. They enrolled 46 patients who were comatose after cardiac arrest and 48 healthy age-matched control participants (mean age, 40.8 ± 16.7 years) in the study. The control subjects had no history of neurologic or psychiatric disorder and were not taking psychoactive medications.
Structural and functional MRI (fMRI) exams were performed at a mean 12.6 days (± 5.6 days) after cardiac arrest on one of three 3-tesla scanners (Tim Trio, Siemens Healthineers; Discovery MR750 and Signa HDxt, GE Healthcare). MRI protocols included a 3D T1-weighted sequence, fluid-attenuated inversion recovery (FLAIR), and diffusion-weighted imaging (DWI). Functional T2-weighted blood oxygen level-dependent (BOLD) images for resting-state fMRI were acquired through 2D gradient-echo echo planar imaging.
The fMRI scans focused on specific networks in the brain, including the default mode network, which is active when a person is not engaged in a specific task, and the salience network, which consists of a collection of brain regions that select which stimuli are deserving of one's attention.
"Multimodality MRI is an immensely valuable approach to explore changes in tissue structure, physiology, and function that can support classification in heterogeneous populations such as this one," Stevens said.
To better gauge cardiac arrest patient outcomes, the researchers used the Cerebral Performance Category scoring method to validate the level of brain function. Scores range from 1 to 5, with 1 meaning good cerebral performance and alertness and 5 meaning brain death. Patients with scores of 1 or 2 were deemed to have a favorable outcome, while those with scores of 3 or more had an unfavorable outcome.
Predictable outcomes
Stevens and colleagues found that at the 12-month mark, 11 patients (24%) had a favorable outcome and 35 patients (76%) had unfavorable outcomes. The most significant factors for a favorable outcome were younger age, presence of ventricular fibrillation, and out-of-hospital cardiac arrest. FLAIR and DWI scores were significantly higher in patients with unfavorable outcomes than in patients with favorable outcomes in all brain regions.
| Favorable outcome differentiators | |||
| Favorable outcome | Unfavorable outcome | p-value | |
| No. of subjects | 11 | 35 | -- |
| Mean age | 38.1 years (± 18.7) | 53.0 years (± 15.3) | 0.025 |
| No. of out-of-hospital cardiac arrests | 11 (100%) | 24 (68.6%) | 0.044 |
| No. with ventricular fibrillation | 8 (72%) | 12 (34%) | 0.038 |
| FLAIR scores | 5.5 (± 4.1) | 14.6 (± 8.5) | 0.0001 |
| DWI scores | 7.3 (± 4.6) | 17.9 (± 11.3) | 0.0001 |
Regarding connectivity between the brain networks, one key predictor of outcomes was the interaction between the default mode and salience networks. Normally, as the default mode network becomes more active, the salience network becomes less active and vice versa.
Patients with favorable outcomes had greater preservation of connectivity within the default mode network (p = 0.002) and higher levels of connectivity between the salience and default mode networks (p < 0.001) than patients with unfavorable outcomes.
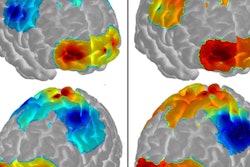
 Representative default mode network resting BOLD maps in control subject (left), patient with favorable outcome (center), and patient with unfavorable outcome (right) overlaid onto axial standard Montreal Neurological Institute (MNI) template. The posterior cingulate (MNI: 45, 37, 49) was seeded and voxels with Pearson correlations greater than 0.6 are shown in red-yellow. Image courtesy of Radiology.
Representative default mode network resting BOLD maps in control subject (left), patient with favorable outcome (center), and patient with unfavorable outcome (right) overlaid onto axial standard Montreal Neurological Institute (MNI) template. The posterior cingulate (MNI: 45, 37, 49) was seeded and voxels with Pearson correlations greater than 0.6 are shown in red-yellow. Image courtesy of Radiology."The distribution and magnitude of tissue signal change on FLAIR and on DWI were both directly linked to the probability of recovery," Stevens said. "However, the changes in network functional connectivity that we identified were stronger outcome predictors."
Stevens and colleagues are now enrolling patients in a prospective observational cohort to map recovery probabilities onto specific phenotypic, neuroimaging, neurophysiologic, and molecular features. The goal is to personalize postcardiac-arrest resuscitation and rehabilitation.
"The results are extremely promising and we intend to validate them in a larger sample," he said. "Following this validation phase, we envision that we could use these functional connectivity markers to guide not only prognostication, but also treatment allocation in clinical trials."