Which MR imaging sequence used with whole-body fluorocholine-PET/MRI is most proficient at detecting metastases and staging patients with prostate cancer? Canadian researchers put four sequences through their paces in a study published online October 17 in the American Journal of Roentgenology.
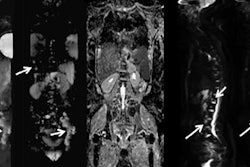
The group concluded that the gadolinium-enhanced T1-weighted volumetric interpolated breath-hold exam (VIBE) was the best of the four sequences. With a total scan time of approximately 88 seconds and the ability to identify 97% of all conspicuous lesions, gadolinium-enhanced T1-weighted VIBE also proved the most time-efficient sequence.
"PET/MRI protocols for staging of patients with high-risk prostate cancer need to be tailored to maximize the benefit of MRI. ... To maximize patient comfort and clinical throughput and to minimize cost, this should be performed with pulse sequences that will result in the best lesion conspicuity in the shortest scan time possible," wrote lead author Dr. Ur Metser and colleagues from Princess Margaret Hospital in Toronto.
Since the introduction of PET/MRI, researchers have explored how to apply the best of both modalities to a range of clinical applications. While MRI alone can provide important information about the location of prostate cancer and the extent of the disease, whole-body MRI "as an adjunct to whole-body PET in the detection of nodal and distant metastases is not well-established," the authors wrote.
"The optimal whole-body PET/MRI protocol would incorporate MRI sequences that contribute the most to lesion localization and characterization, while keeping scan time to a minimum," they added.
Metser and colleagues therefore decided to compare the following four whole-body MRI protocols, measuring the ability of each to detect lesions and recording the amount of time required to perform each one:
- Coronal T1-weighted 3D Dixon (1 minute, 25 seconds)
- Coronal T2-weighted turbo inversion-recovery magnitude (TIRM) (15 minutes, 7 seconds)
- Whole-body diffusion-weighted imaging (DWI) (16 minutes, 33 seconds)
- Gadolinium-enhanced T1-weighted VIBE (1 minute, 28 seconds)
For the study, the group analyzed 58 consecutive patients with previously untreated, biopsy-proven high-risk prostate cancer between January 2014 and July 2016. The subjects had 77 confirmed metastases: 41 regional nodal metastases, 25 extraregional nodal sites, and 11 skeletal metastases.
All patients were scanned on one of two imaging platforms: 10 patients underwent whole-body fluorocholine-PET/MRI scans (Biograph mMR, Siemens Healthineers), while 48 underwent fluorocholine-PET/CT scans (Biograph mCT 40, Siemens) and whole-body MRI on a 3-tesla (Magnetom Skyra, Siemens) scanner.
Histopathologic results or clinical and imaging follow-up (or both) served as the reference standard. Most of the scans were performed on the same day, and two radiologists assessed metastatic lesion conspicuity on a scale of 0 to 3.
The researchers found that gadolinium-enhanced T1-weighted VIBE achieved the best detection rate (97%) for lesions with a conspicuity score of 1 or greater, followed by whole-body DWI (95%) and TIRM (95%). The only statistically significant difference was between the gadolinium-enhanced T1-weighted VIBE and T1-weighted 3D Dixon sequences (p = 0.0285). In addition, both the gadolinium-enhanced T1-weighted VIBE (p < 0.0001) and whole-body DWI (p = 0.0011) sequences were better on a statistically significant basis than T1-weighted 3D Dixon in assessing lesions and determining a moderate-to-high conspicuity score of 2 or greater.
| Prostate lesion detection rates and conspicuity by MRI sequence | ||||
| Gadolinium-enhanced T1-weighted VIBE | Whole-body DWI* | Turbo inversion-recovery magnitude | T1-weighted 3D Dixon | |
| Lesion detection rate | 97% | 95% | 95% | 88% |
| Moderate-to-high conspicuity | 92% | 90% | 88% | 62% |
The findings also have implications for PET's role: Metser and colleagues suggested that the results "are likely to be applicable to other radiotracers, including prostate-specific membrane antigen," even though only fluorocholine was used in this study.



.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=100&q=70&w=100)


.fFmgij6Hin.png?auto=compress%2Cformat&fit=crop&h=167&q=70&w=250)