Obesity can change more than the size of your waistline. In a new study published online April 23 in Radiology, Dutch researchers used MR images to link greater levels of body fat to changes in the brain's form and structure, particularly with smaller volumes of gray matter.
The effect of the alterations is still to be determined, but the brain regions most affected in men and women are known to be centers for the feeling of reward from food-related stimuli. That activity could make weight loss more challenging for some individuals. The researchers also correlated gender as an important factor in determining the percentage of a person's body fat and the size of specific brain structures.
"In our study, we showed that sex differences are manifest regarding negative associations of total body fat percentage with regional subcortical gray matter volumes, including the globus pallidus and caudate nucleus, which have been associated with the reward circuitry of food-related stimuli," wrote the researchers led by Dr. Ilona Dekkers from Leiden University Medical Center in the Netherlands.
Obesity epidemic
It is no secret that obesity has increased to epidemic proportions in many developed countries. While excess body weight has led to an increased prevalence of cardiovascular disease and type 2 diabetes, it also has paralleled a rise in adverse neurological conditions, such as cognitive decline and dementia. In fact, previous postmortem studies have shown higher levels of beta-amyloid plaques and tau protein -- two leading indicators of Alzheimer's disease -- in obese elderly patients compared with nonobese older patients.
Other MR imaging studies have linked body mass index to lower gray matter volume and white matter integrity, while other research has suggested that structural differences in certain brain regions could play a role in regulating one's eating habits.
Taking it one step further, the Dutch researchers hypothesized that "lower volume of brain regions or decreased microstructural integrity of tracts involved in the neuronal regulation of the food-reward circuitry might also be associated with obesity."
To test their theory, they perused data of more than 500,000 participants in the U.K. Biobank study, which began in 2006 to learn more about the genetic and environmental factors that influence disease. From that pool, 12,087 participants with a mean age of 62 (± 7.3 years; range, 45 to 76 years) met the inclusion criteria. Of those subjects, 6,381 (53%) were women and 5,706 were men (47%). Brain scans were acquired on a 3-tesla system (Magnetom Skyra, Siemens Healthineers) with a standard 32-channel radiofrequency receiver head coil.
MRI protocol
The brain imaging protocol included 3D T1-weighted diffusion-tensor imaging (DTI), which acquired fractional anisotropy measurements to determine white matter integrity and water molecule diffusion. In addition to total body fat calculations, volumetric measures were performed to gauge overall brain volume, gray and white matter volumes, subcortical gray matter structure volumes, and regional cortical volumes.
In comparing the two genders, the researchers found that among men, 5.5% more total body fat was associated with 27 mm3 smaller globus pallidus volume. With women, 6.6% greater total body fat percentage was associated with 11.2 mm3 smaller globus pallidus volume. The association between total body fat and globus pallidus volume was significantly lower in women than in men (p = 0.001).
Regarding white matter evaluation, higher total body fat was positively associated with greater global fractional anisotropy values (directional coherence of water molecule diffusion) but negatively associated with mean diffusivity (magnitude of water molecule diffusion). This finding would indicate that body fat percentage, as a measure of general obesity, is associated with a higher coherence and a lower magnitude of water diffusion.
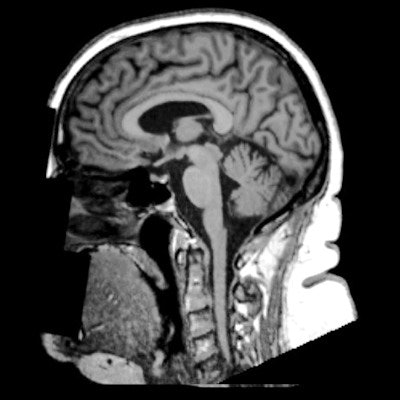
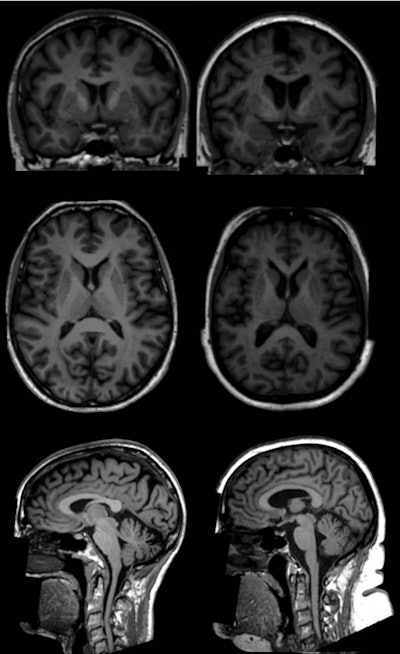 T1-weighted brain MR images show examples (coronal, top; axial, middle; and sagittal, bottom) of two women (age 65) in the U.K. Biobank study. One subject has a body fat percentage of 13% (left), while the other woman has a body fat percentage of 49% (right). MR images show lower volumes of subcortical gray matter structures in the individual with higher total body fat percentage (right). Images courtesy of Radiology.
T1-weighted brain MR images show examples (coronal, top; axial, middle; and sagittal, bottom) of two women (age 65) in the U.K. Biobank study. One subject has a body fat percentage of 13% (left), while the other woman has a body fat percentage of 49% (right). MR images show lower volumes of subcortical gray matter structures in the individual with higher total body fat percentage (right). Images courtesy of Radiology.The smaller volume of gray matter could mean a loss of neurons, while changes to the white matter could adversely affect the transmission of signals within brain networks, the researchers noted. Given that gray matter is known to play a role in the brain's food-reward circuitry, the alterations could make it more difficult for obese people to control their weight, Dekkers and colleagues posited.
"For future research, it would be of great interest whether differences in body fat distribution are related to differences in brain morphological structure, as visceral fat is a known risk factor for metabolic disease and is linked to systemic low-grade inflammation," added senior author Dr. Hildo Lamb, PhD, director of cardiovascular imaging at Leiden University Medical Center, in a prepared statement.



















