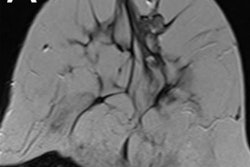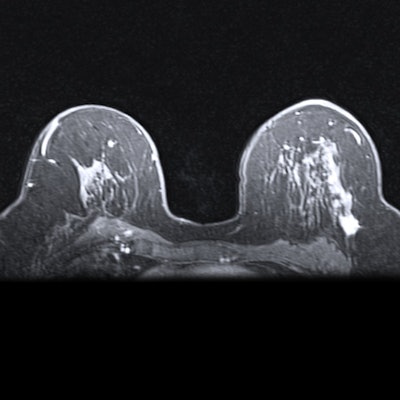
Breast MRI may improve surgical success for women with breast cancer, according to a study published on March 17 in Radiology. Patients who underwent presurgical MRI had fewer positive surgical margins and repeat surgeries than those who did not.
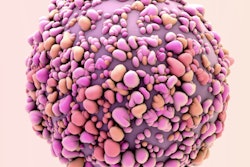
The study compared the surgical outcomes for hundreds of women with biopsy-confirmed ductal carcinoma in situ (DCIS). The findings demonstrate MRI's strength as a breast cancer diagnostic and staging tool and also as one for surgical planning.
"Our results show that preoperative breast MRI is associated with a reduction in the rates of positive resection margin and repeat surgery, without evidence of different initial or overall mastectomy rates," wrote the authors, led by Dr. Ga Young Yoon, PhD, of the University of Ulsan College of Medicine in Gangneung, South Korea.
The study included 541 women who were diagnosed with ductal carcinoma in situ at a university hospital between January 2012 and December 2016. All women had mammography and ultrasound-guided breast core needle biopsy. However, 79.5% of the patients also underwent presurgical MRI.
Presurgical MRI identified eight size discrepancy lesions and 67 additional suspicious lesions. The suspicious lesions were followed up with surgical excision, MRI-directed ultrasound with biopsy, and long-term monitoring.
Furthermore, presurgical MRI changed the surgery plan for 57 women. In 49% of surgical changes, the women received contralateral breast excision. Another 30% underwent wider excision, and 21% changed from breast-conserving surgery to mastectomy.
Women who underwent MRI had better surgery outcomes, the authors noted. They were less likely to have a positive resection margin at initial surgery and lower odds of needing additional surgery. Presurgical MRI also did not significantly change the rates at which women underwent mastectomies.
While presurgical MRI had benefits, the researchers considered 46% of the surgery changes to be unnecessary. Nine unnecessary changes were for high-risk lesions, including for five women who were diagnosed at an additional biopsy and underwent surgery and four women who were diagnosed at surgical excision without an ultrasound-guided core-needle biopsy.
"The rate of unnecessary surgical planning changes was relatively high in this study because 19 of the additional suspicious lesions were excised surgically without preoperative biopsy, and high-risk lesions confirmed by MRI-direct [ultrasound] and [core-needle biopsy] were included in the unnecessary change group," the authors wrote.
They also found significant differences between women who benefited and didn't benefit from presurgical MRI. Women who benefited from presurgical MRI had low nuclear grade, progesterone receptor positivity, and human epidermal growth factor receptor 2 negativity.
"Most women with a large lesion underwent mastectomy as initial treatment and were considered as the no benefit group," the authors wrote. "Thus, women with a relatively smaller lesion may remain in the benefit group."
Despite its limitations, presurgical MRI still appears to be a helpful surgical planning tool for women with DCIS, the authors concluded.
"Our results show that preoperative breast MRI is beneficial in the surgical planning in women with ductal carcinoma in situ confirmed by using [ultrasound]-guided core-needle biopsy," the authors wrote. "Preoperative breast MRI is helpful for depicting additional malignancy and reducing the rates of positive resection margin and repeat surgery, without evidence of a different mastectomy rate."