It might be wise to shift the main focus of research into gadolinium deposition from the brain to the skin and its innervation, particularly in light of the growing evidence from the latest animal studies, a leading European researcher has proposed.
"In times of scarce scientific resources, it is important to focus on the investigation of side effects that are most probable," noted Prof. Dr. Alexander Radbruch, chair of diagnostic and interventional neuroradiology at Rheinische Friedrich Wilhelms University Bonn in Germany, in an editorial published online by Radiology on August. 18
He thinks it is vital to consider the following warnings: nephrogenic systemic fibrosis can manifest in the skin after injection of linear gadolinium-based contrast agents (GBCAs) for MRI; gadolinium concentrations are among the highest in the skin (for the linear GBCA gadodiamide) and in the peripheral nerves; and some patients report peripheral pain after GBCA injection.
Furthermore, an important study about gadolinium retention in the central and peripheral nervous system was also published by Radiology on August 18. First author Safia M. Alkhunizi from the American University of Beirut, Lebanon, and colleagues concluded that the linear GBCA gadodiamide induced hyperalgesia in the hind paws of mice, Radbruch explained.
To illustrate his point, Radbruch recounted an old joke about the so-called streetlight effect. The joke is still popular among scientists today.
"When a drunk man is crawling at night under a streetlight looking for his wallet, a policeman asks the man if he is sure that he dropped the wallet under the streetlight. The drunk man answers that he probably dropped the wallet in the park, but that the light is better under the streetlight," he wrote. "Without taking it too seriously, radiologists might have acted like the drunk man in the old joke when it comes to gadolinium deposition in the brain."
 Have radiologists been influenced too much by the streetlight effect when it comes to gadolinium deposition?
Have radiologists been influenced too much by the streetlight effect when it comes to gadolinium deposition?Small fiber neuropathy
Radbruch's own group has published a related paper, "Is Small Fiber Neuropathy Induced by Gadolinium-Based Contrast Agents?" in the August edition of Investigative Radiology.
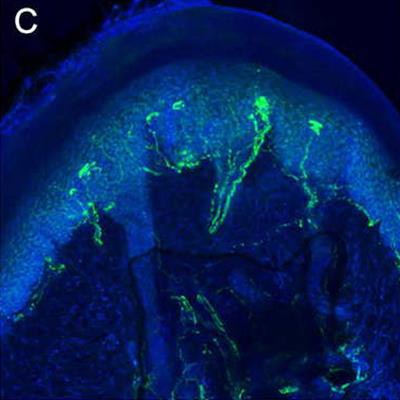
The team found a significant decrease of intraepidermal nerve fiber density (IENFD) four weeks after a single injection of all GBCAs (1 mmol/kg BW) in the footpads of mice. The IENFD decrease was significantly higher after injection of linear compared with macrocyclic GBCAs. In addition, mice injected with linear GBCAs showed a notable increase of terminal axonal swellings (TASs) per IENFD, whereas macrocyclic GBCAs showed a TAS per IENFD increase that did not reach the level of significance compared with controls.
 The images show small fibers in the skin of footpads of mice following a single injection of a human equivalent dose (1 mmol/kg BW) of saline (A), macrocyclic gadolinium-based contrast agent (GBCA) gadobutrol (B), and nonionic linear GBCA gadodiamide (C), visualized with laser ablation inductively coupled plasma-mass spectrometry. Compared to A, the number of small fibers is slightly reduced in B, while the number of small fibers is strongly reduced in C. Moreover, terminal axonal swellings are visible after the injection of gadodiamide in C. Figure courtesy of Investigative Radiology, derived from Invest Radiol, 2020 Aug;55(8):473-480.
The images show small fibers in the skin of footpads of mice following a single injection of a human equivalent dose (1 mmol/kg BW) of saline (A), macrocyclic gadolinium-based contrast agent (GBCA) gadobutrol (B), and nonionic linear GBCA gadodiamide (C), visualized with laser ablation inductively coupled plasma-mass spectrometry. Compared to A, the number of small fibers is slightly reduced in B, while the number of small fibers is strongly reduced in C. Moreover, terminal axonal swellings are visible after the injection of gadodiamide in C. Figure courtesy of Investigative Radiology, derived from Invest Radiol, 2020 Aug;55(8):473-480.The clinical significance of these findings remains unclear, Radbruch pointed out.
"We urge the scientific community to treat the results of our study with caution," he told AuntMinnieEurope.com. "It remains unclear if and at what dosage the decrease of small fibers in the current animal study can be transferred to humans and if it causes clinical symptoms. It also needs to be emphasized that one of the biggest threats of the current debate remains the avoidance of gadolinium in clinically indicated situations."
However, the results of the current study could explain the neuropathic pain of patients following gadolinium injections, and researchers have an ethical obligation to assess the potential side effects of gadolinium exposure, according to Radbruch.
"Two ways are thinkable for further studies: analysis of big data sets of patients suffering from small fiber neuropathy and prospective studies evaluating skin biopsies in patients prior and after gadolinium exposure. Both study types are challenging since a lot of potential confounders need to be considered," he said.
The results of the recent research should encourage further studies on the reduction of gadolinium or gadolinium-free imaging.
"For example, we plan to reduce the amount of gadolinium in our hospital with the help of artificial intelligence," he concluded. "Regardless of the results of the clinical studies, the reduction of gadolinium with new postprocessing and imaging techniques is definitely the way to move forward."