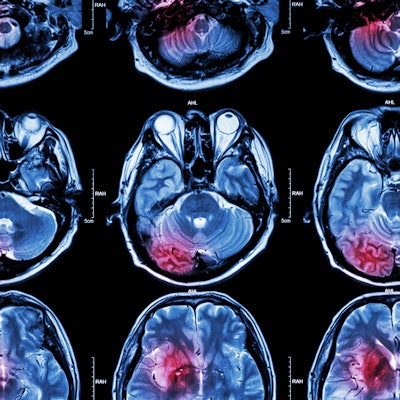
Particular findings on brain MRI appear to be connected to atrial fibrillation in stroke patients -- and perhaps to future cognitive decline, according to a study conducted by Swedish researchers and published September 14 in Neurology.
The study results offer new clues to the causes of atrial fibrillation, wrote a team led by Dr. Lina Rydén of the University of Gothenburg in Sweden.
"We found that atrial fibrillation was associated with a history of symptomatic stroke and several brain pathologic markers, such as large infarcts, lacunes, and silent brain infarcts," the group noted. "Atrial fibrillation was [also] associated with larger white matter hyperintensities volumes in individuals with symptomatic stroke, but not in those without."
Atrial fibrillation has been linked to cognitive decline and dementia, but the mechanisms of the connection aren't well-defined, the authors noted. Using MRI to evaluate brain pathology shows potential for clarifying this association.
"Atrial fibrillation has been associated with stroke, dementia, and mortality, but the mechanisms behind these associations, in the absence of cardiac embolism, are not clear," the group wrote.
Rydén and colleagues investigated whether atrial fibrillation is connected to cerebrovascular conditions beyond symptomatic stroke such as undiagnosed strokes, cerebral microbleeds, white-matter hyperintensities, and lacunes. Their study data came from the Gothenburg H70 Birth Cohort Studies and included 776 70-year-olds who underwent a brain 3-tesla MRI exam between 2014 and 2017. The exams used a protocol that included T1, T2, fluid-attenuated inversion recovery (FLAIR), T2*, and diffusion-weighted imaging sequences.
Atrial fibrillation and symptomatic stroke diagnoses were based on patient reports, electrocardiogram results, and data from Sweden's National Patient Register (NPR); stroke diagnosis, on patient (or patient helper) report, interviews with nurses or physicians, and NPR information; brain infarcts and cerebral microbleeds on radiologist assessment; and white-matter hyperintensities on MRI. Patients were also assessed for dementia according to the Diagnostic and Statistical Manual of Mental Disorders (DSM-III-R) using information gleaned from psychiatric exams.
Of the 776 study participants, 65 (8.4%) had atrial fibrillation. The researchers noticed that atrial fibrillation was associated with the MRI findings illustrated in the following table.
| Odds ratios for atrial fibrillation related to MRI findings | ||||
| Finding | Odds ratio (unadjusted*) | p-value (unadjusted*) | Odds ratio (adjusted*) | p-value (adjusted*) |
| Large infarct | 7.9 | < 0.001 | 5 | 0.007 |
| Lacune | 3.4 | < 0.001 | 2.7 | 0.008 |
| Silent brain infarct | 4.6 | < 0.001 | 3.5 | 0.001 |
The researchers also noted that in patients with symptomatic stroke, those with atrial fibrillation had larger white-matter hyperintensity volumes compared with those without the condition (0.0137 mL/total intracranial volume vs. 0.0043 mL/total intracranial volume), and that atrial fibrillation appeared linked to cerebral microbleeds in the frontal lobe.
It's possible that the study results could improve patient care by refining stroke patient treatment strategies and helping clinicians predict patients' longer-term outcomes. But that will require more study.
"Further research is needed to establish whether cerebrovascular MRI markers can be added to current treatment guidelines to further personalize anticoagulant treatment in atrial fibrillation patients and to further characterize the pathogenetic processes underlying the associations between atrial fibrillation and cerebrovascular diseases, as well as dementia," the group concluded.