VIENNA - Preoperative MRI helps surgeons predict whether colorectal cancer structures -- for example, the omentum and ovaries, the pelvic peritoneum, or the ileum -- can be effectively removed, according to research presented at ECR 2023.
Using MRI in this way could not only help with surgery planning but also help manage patient expectations about surgery outcomes, especially if the surgeon suspects that the patient may have a permanent stoma post procedure or need additional specialists to be in attendance, said presenter Dr. Max Lahaye of the Netherlands Cancer Institute in Amsterdam.
"[We found that MRI] has a high positive predictive value for predicting stoma post CRS-HIPEC [cytoreductive surgery and heated intra-peritoneal chemotherapy] and whether additional specialists will be needed [during surgery]," he said.
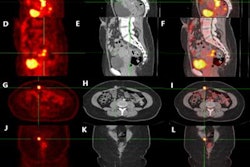
When it comes to treating colorectal cancer with surgery, multidisciplinary teams of clinicians evaluate whether a patient is a good candidate. Surgeons then decide, using clinical and radiological findings, what structures will need to be removed. There are a variety of ways to detect peritoneal metastases before surgery, including laparoscopy, laparotomy (both of which are invasive), and CT. But MRI is the most accurate tool and has the advantage of being noninvasive and relatively inexpensive, Lahaye said, citing data from a 2020 study published in European Radiology.
| Modality performance comparison for detecting peritoneal metastases | ||
| Modality | Sensitivity | Specificity |
| MRI | 92% | 84% |
| PET/CT | 79% | 90% |
| CT | 68% | 88% |
For this research, Lahaye's group included 29 colorectal cancer patients with peritoneal metastases who had a preoperative MRI before undergoing CRS-HIPEC. Three surgeons reviewed the MRI findings to predict the probability of complete resection of 204 abdominal structures; the most common structures were the omentum and ovaries, the pelvic peritoneum, and the ileum. After surgery, the team reviewed histopathological reports to assess surgical success.
The group found that imaging patients preoperatively with MRI produced the following results:
- Intraclass correlation among the three surgeons of 0.92.
- Viable tumor tissue was removed in 75% of all cancerous tissue.
- Overall positive predictive values for the resected structures ranged from 80.8% to 100%.
- Negative predictive values for the resected structures ranged from 50% to 100%.
It's apparent that MRI helps surgical planning and patient management of colorectal cancer treatment, and that there's high agreement among surgeons for predicting whether the surgery will be a success. But the percentage of success could be higher, Lahaye and colleagues concluded in their abstract on the findings.
"Surgeons can accurately predict the resectability of certain anatomical structures and variables that could be useful in surgical planning and patient expectation management based on MRI findings," the group wrote. "However, more tools are necessary perioperatively to distinguish benign from malignant lesions since 25% of the resected structures were not malignant."