Chemotherapy appears to negatively affect breast cancer survivors' cognitive function, according to research presented at the recent International Society for Magnetic Resonance in Medicine (ISMRM) 2025 meeting in Honolulu.
The changes seem to be linked to alterations in brain connectivity, a team led by Khulan Khurelsukh, MD, of Chang Gung University in Taiwan, reported. The findings could influence how breast cancer survivors are tracked after treatment.
"This research impacts clinicians and breast cancer survivors by identifying connectivity indicators for cognitive function," the group wrote. "It raises new questions about personalized interventions, allowing for customized strategies to mitigate cognitive decline and enhance the quality of life for patients after chemotherapy."
Breast cancer treatments can impact women's memory, thought processing speed, and executive function, the investigators explained, noting that up to 75% of patients experience chemotherapy-related cognitive impairment (CRCI). Factors that influence CRCI include an individual's age, genetics, level of inflammation, and psychological stress, they wrote.
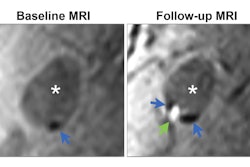
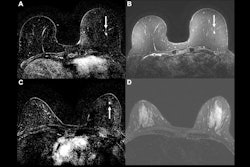
Khurelsukh and colleagues used functional MRI to investigate changes in resting-state functional connectivity and structural networks in women who had undergone chemotherapy for breast cancer. They also examined any associations with cognitive performance after chemotherapy. The group did this via analysis of mean regional homogeneity (mReHo) and mean fractional amplitude of low-frequency fluctuations (mfALFF) values and results from Network-Based Statistics (NBS) and Graph Theory Analysis (GAT) in breast cancer patients before and after chemotherapy compared with healthy controls.
The study included 28 matched pairs in a chemotherapy group and 27 matched pairs in a healthy control group; all participants underwent a 3-tesla MRI exam at baseline and at one-year follow-up. The team also assessed each individual with the Patient Health Questionnaire-9 (PHQ-9), Hospital Anxiety and Depression Scale-Anxiety subscale (HADS-A), Functional Assessment of Cancer Therapy Cognitive Version 3 (FACT-Cog), and Digit Symbol Substitution (DSS).
The authors found that breast cancer patients' anxiety scores decreased after chemotherapy, "indicating reduced psychological distress," but also that "FACT-Cog scores revealed a notable postchemotherapy cognitive decline, especially in memory, with greater impairment compared to controls over a six-month follow-up."
They also reported the following:
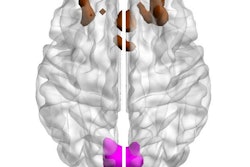
- Breast cancer patients treated with chemotherapy showed increases in frontal gyri but decreases in the left lingual gyrus and bilateral parahippocampal gyrus -- a finding that implies disruptions in visual and memory processing.
- The study showed significant brain network organization changes in the postchemotherapy group.
- Weaker structural connections in areas associated with attention and sensory-motor functions were identified in breast cancer patients both before and after chemotherapy compared to controls.
The results "highlight the relationship between neural changes and cognitive decline, particularly in subjective cognitive complaints, providing valuable insights into the neural mechanisms underlying chemotherapy-related cognitive impairment," according to Khurelsukh and colleagues.
"[Our] findings support the hypothesis that chemotherapy induces widespread connectivity reorganization in cognitive and sensory networks, contributing to cognitive challenges in breast cancer survivors," they concluded.