Radiation therapy (RT) following chemotherapy carries the risk of future complications for children and young adults with Hodgkin's lymphoma, but results published online May 29 in the Journal of Clinical Oncology show that patients who received radiotherapy after chemo had a lower risk of cancer recurrence.
The study findings reinforce the validity of the current standard of care, a combination of multiagent chemotherapy and low-dose involved-field radiotherapy, individualized to each patient.
Clinical Trial 5942, conducted by the Children's Cancer Group, was initiated in 1995 to evaluate whether low-dose involved-field radiation therapy improved event-free survival for patients who achieved a complete response after undergoing chemotherapy. The underlying question to be answered was whether radiation, with its potentially devastating aftereffects, could be safely eliminated from the treatment regimen of young Hodgkin's lymphoma patients.
Patients who had an initial complete response to chemotherapy were randomly assigned to either not have any additional treatment or to have low-dose involved-field radiation therapy. The radiation therapy was administered in daily fractions of 1.75 Gy, for a total dose of 21 Gy.
Although trial enrollment was closed in 1998 because patients receiving chemotherapy only were having a higher level of relapse compared to patients receiving chemoradiotherapy, 498 patients qualified to be evaluated.
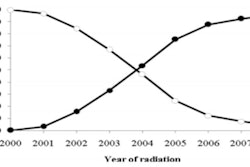
Lead author Dr. Suzanne Wolden, a radiation oncologist at Memorial Sloan-Kettering Cancer Center, and co-investigators reported findings based on data acquired through March 2007. There was no difference in overall survival; however, the 233 patients in the chemoradiotherapy group had a cancer-free survival rate of 91.2%, compared with 82.9% for the 265 patients in the chemotherapy-only group.
The clinical trial had an original enrollment of 826 patients, 326 of whom did not completely respond to the initial chemotherapy treatment. A total of 54 patients had died by March 2007; 90% died from progressive disease or from toxicities associated with its treatment.
The vast majority of relapses among the 498 patients who were randomized and followed occurred within four years of treatment. Nineteen patients in the chemoradiotherapy group relapsed, 79% within the first four years. Forty-three patients in the chemotherapy-only group relapsed, all but two patients within this time frame. Independent predictors of relapse for all 826 patients were bulk disease and B symptoms, such as significant fever, Pel-Ebstein fever, night sweats, and unintentional weight loss of more than 10%.
Observing that treatment with involved-field radiation therapy prevents nine relapses for every 100 patients who achieve a complete response to initial therapy, the authors stressed that the risk of this treatment must be assessed on a patient-by-patient basis. Risks vary dramatically depending on the age, sex, and specific characteristics and location of the cancer. When an aggressive chemotherapy regimen is prescribed, it may be possible to reduce the radiation dose for a patient.
Dr. Sarah Donaldson, professor of radiation oncology at Stanford University Medical Center, wrote in an accompanying editorial that curative treatment must be balanced with the quality of life that young survivors will have and their ability to lead normal and productive lives as adults. A high cure rate with the least amount of treatment-induced toxicity is being achieved with limited cycles of nontoxic chemotherapy agents combined with low-dose, limited-volume radiotherapy in a risk-based profile.
Decreasing therapy should be done with caution, she advised, stating that the balance between cure and toxicity is a delicate one. Today, 90% of all patients with pediatric Hodgkin's lymphoma survive. The remaining 10% represent the unsolved challenge for the cancer specialists who treat them.