Ultrasound-guided thermal ablation techniques are safe and effective in treating patients with secondary hyperparathyroidism, suggest findings published January 7 in Radiology.
Researchers led by Yang Liu, MD, from the Chinese PLA General Hospital in Beijing found that both microwave ablation (MWA) and radiofrequency ablation (RFA) reduced parathyroid hormone levels along with calcium, phosphorus, and alkaline phosphate levels.
“At the end of the follow-up period, 85.1% of ablation-treated participants had achieved the target [parathyroid hormone] level,” Liu and co-authors wrote. “Treatment with ultrasound-guided MWA and RFA was generally well tolerated.”
In recent years, researchers have been exploring the efficacy and safety of image-guided ablation techniques. Previous reports indicate that both MWA (which uses microwaves) and RFA (which uses radio waves) fit both criteria. And interest in applying these interventional techniques in patient care continues to rise.
However, the investigators noted that ablation outcomes in patients with secondary hyperparathyroidism have not been well characterized.
Liu and colleagues studied how ultrasound-guided MWA and RFA affect parathyroid hormone, calcium, phosphorus, and alkaline phosphatase levels. They also assessed the safety of these treatments in secondary hyperparathyroidism patients.
The study included 215 patients with a median age of 53 years who had confirmed secondary hyperparathyroidism between 2017 and 2022. The target parathyroid hormone level was set to less than or equal to 585 pg/mL. The researchers studied parathyroid hormone, calcium, phosphorus, and alkaline phosphate levels before ablation and time points for follow-up assessments after ablation (these included two hours, one day, one month, three months, six months, and then every six months after that). They also developed a risk-based prediction model based on independent risk factors and their corresponding parameter estimates.
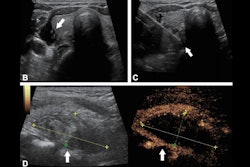
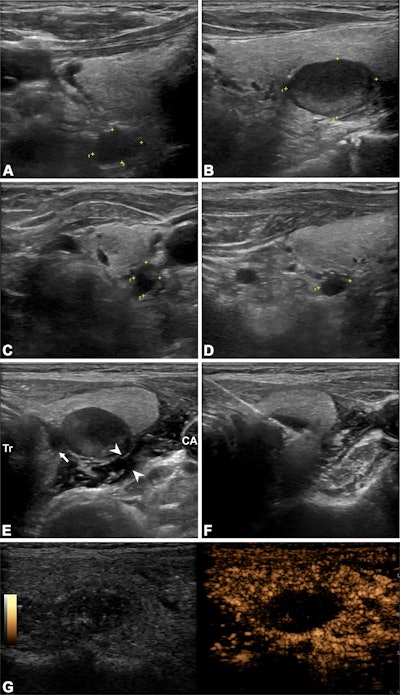 Ultrasound images depict a 63-year-old man who underwent radiofrequency ablation (RFA) for the treatment of secondary hyperparathyroidism. (A–D) 2D images show four hyperplastic parathyroid glands on the right and left sides (marked with crosshairs). The numbers near the crosshairs represent the number of measured trails. (E) Ultrasound-guided infusion of isolation fluid (arrowheads) around the hyperplastic parathyroid gland to protect vital organs such as the trachea (Tr), carotid arteries (CA), and recurrent laryngeal nerve pathway area (arrow). F) Ultrasound-guided RFA of the hyperplastic parathyroid gland. (G) Immediate postoperative contrast-enhanced ultrasound shows no contrast enhancement in the ablation area. The ablation procedures for the other three parathyroid glands were the same as those described above. Image courtesy of the RSNA,
Ultrasound images depict a 63-year-old man who underwent radiofrequency ablation (RFA) for the treatment of secondary hyperparathyroidism. (A–D) 2D images show four hyperplastic parathyroid glands on the right and left sides (marked with crosshairs). The numbers near the crosshairs represent the number of measured trails. (E) Ultrasound-guided infusion of isolation fluid (arrowheads) around the hyperplastic parathyroid gland to protect vital organs such as the trachea (Tr), carotid arteries (CA), and recurrent laryngeal nerve pathway area (arrow). F) Ultrasound-guided RFA of the hyperplastic parathyroid gland. (G) Immediate postoperative contrast-enhanced ultrasound shows no contrast enhancement in the ablation area. The ablation procedures for the other three parathyroid glands were the same as those described above. Image courtesy of the RSNA,
Of the total patients, 183 (85.1%) achieved target parathyroid hormone levels. Compared with baseline levels, the researchers reported an 85.9%, 6.3%, 15.3%, and 37.4% reduction in parathyroid hormone, calcium, phosphorus, and alkaline phosphate levels at 24 months after ablation, respectively.
One patient experienced persistent hoarseness, while 74 experienced severe hypocalcemia. After adjustments, the researchers found that the following predictors were tied to treatment failure: pre-ablation parathyroid hormone level (adjusted odds ratio [OR], 3.78; p = 0.03), maximum tumor volume (adjusted OR, 5.02; p = 0.003), and the number of glands ablated (adjusted OR, 0.32; p = 0.046).
Finally, the prediction model showed good discriminatory ability in the development and validation cohorts. This included area under the receiver operating characteristic curve (AUROC) values of 0.78 for the development cohort and 0.73 for the validation cohort.
Liu and colleagues called for prospective controlled study designs to be considered for future studies to further compare ultrasound-guided ablation and a surgical procedure at the same time.
In an accompanying editorial, Joseph Gemmete, MD, from the University of Michigan in Ann Arbor wrote that such techniques present “an exciting, minimally invasive option” for managing secondary hyperparathyroidism in patients with chronic kidney disease.
“Although further research is needed to confirm its long-term efficacy and safety, this technique has the potential to transform [secondary hyperparathyroidism] management, expanding treatment options for patients who face substantial challenges with current therapeutic approaches,” Gemmete wrote.
The full study can be accessed here.