Ultrasound features of nonmass breast lesions differ across clinical indications, according to findings published October 7 in Radiology.
Researchers led by Vivian Park, MD, PhD, from Severance Hospital, Yonsei University College of Medicine in Seoul, South Korea, found that these imaging features are also influenced by factors such as mammographic findings, symptoms, and lesion laterality.
“Across the clinical indication subgroups, [and] the areas under the receiver operating characteristic curve of … BI-RADS, assessments for diagnosing malignant nonmass lesions at ultrasound were lowest in women undergoing preoperative ultrasound for newly diagnosed, current breast cancer,” Park and colleagues wrote.
Awareness of nonmass lesions is growing among radiologists, with the upcoming sixth edition of BI-RADS including recommendations for reporting clinical indications -- which may include nonmass lesions as a new category, the team noted. Ultrasound is used for these lesions, which appear similar to asymmetries at mammography or nonmass enhancement at either MRI or contrast-enhanced mammography.
However, Park and co-authors noted that the diagnostic performance of breast ultrasound for these lesions is not well validated. The team evaluated and compared the imaging features and diagnostic performance of ultrasound for nonmass lesions across different clinical indications, including assessment of whether nonmass lesions are found across screening, diagnostic workup, and diagnostic current breast cancer exams.
The retrospective study included 1,152 lesions in 1,152 women with an average age of 48 years. The women underwent ultrasound-guided biopsy between 2014 and 2021.
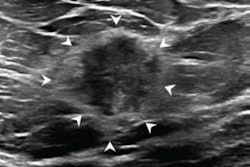
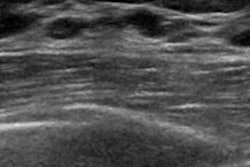
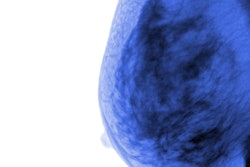
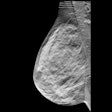
 Images in a 53-year-old woman with a nonmass lesion detected at preoperative evaluation of newly diagnosed right breast cancer. (A) T1-weighted early contrast-enhanced axial preoperative MRI scan shows focal nonmass enhancement in the left upper-outer breast (arrow). (B) Transverse and (C) longitudinal ultrasound images show a nonmass lesion (arrows, crosses) in the left upper-outer breast with several adjacent small cysts (arrowheads). (D) A T2-weighted fat-suppressed axial MRI scan also shows a small cyst (arrowhead) in the corresponding area. (E) Left mediolateral oblique mammogram shows heterogeneously dense breast tissue without findings suspicious for cancer. The lesion was confirmed to be ductal carcinoma in situ with ultrasound-guided core biopsy and subsequent surgery.RSNA
Images in a 53-year-old woman with a nonmass lesion detected at preoperative evaluation of newly diagnosed right breast cancer. (A) T1-weighted early contrast-enhanced axial preoperative MRI scan shows focal nonmass enhancement in the left upper-outer breast (arrow). (B) Transverse and (C) longitudinal ultrasound images show a nonmass lesion (arrows, crosses) in the left upper-outer breast with several adjacent small cysts (arrowheads). (D) A T2-weighted fat-suppressed axial MRI scan also shows a small cyst (arrowhead) in the corresponding area. (E) Left mediolateral oblique mammogram shows heterogeneously dense breast tissue without findings suspicious for cancer. The lesion was confirmed to be ductal carcinoma in situ with ultrasound-guided core biopsy and subsequent surgery.RSNA
Malignancy rates were 10.4% for screening, 43.4% for diagnostic workup, and 40.1% for diagnostic current breast cancer, respectively.
The researchers also reported the following ultrasound imaging features significantly associated with malignancy: lesion size, hypoechogenicity, hyperechogenicity, segmental distribution, abnormal duct changes, calcifications, posterior shadowing, and the absence of multiple small cysts (all p < 0.05). The screening subgroup had the lowest positive predictive value (PPV) at 0% to 60%.
Clinical BI-RADS assessments showed a significantly lower area under the curve (AUC) in the diagnostic current breast cancer subgroup (0.72) compared with the screening (0.89) and diagnostic workup (0.88) subgroups (both p < 0.001). And nonmass lesions in the screening subgroup that did not have suspicious ultrasound imaging features for cancer and mammographic findings had malignancy rates of 2.5% to 2.7%.
Finally, the PPVs of ultrasound features varied by mammography findings, symptoms, and lesion laterality, respectively (all, p < 0.05).
The results provide evidence for integrating clinical context into interpreting nonmass lesions, according to an accompanying editorial written by Baṣak Dogan, MD, from the University of Texas Southwestern Medical Center in Dallas.
“Standardized descriptors in the sixth edition of the BI-RADS ultrasound lexicon, informed by studies such as this one, should help bring greater consistency and precision to nonmass lesion evaluation, ultimately improving patient care while avoiding unnecessary interventions,” Dogan wrote.
Read the full study here.