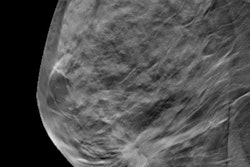
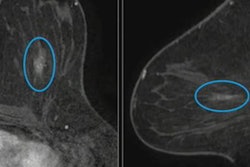
Digital breast tomosynthesis (DBT) could improve screening performance over conventional mammography in younger and older age groups, suggest findings published January 28 in the American Journal of Roentgenology.
DBT showed better cancer detection and recall rates over mammography in women ages 40 to 44 and in women over the age of 75, both age groups being outside the criteria for inclusion in the Tomosynthesis Mammographic Imaging Screening Trial (TMIST).
“What we found surprising was how low the screening performance was for digital mammography in the women 40 to 44, as well as the benefit of lower recall rates for all women in the study,” said lead author Jean Seely, MD, from the Ottawa Hospital in Ontario, Canada.
Before the TMIST study began in 2017, the TMIST Lead-in trial served as a pilot for the full study. This randomized controlled trial, which began in 2014, enrolled women aged 40 and older who were already scheduled for screening mammography. These women were also randomized to either digital mammography or DBT.
However, after the researchers finalized the full TMIST protocol, the study allowed only women aged 45 to 74 at the time of trial entry. This meant that women who participated in the Lead-in trial who were ages 40 to 44 years or 75 years and older were ineligible for transition to the full trial.
Seely and colleagues compared the respective screening performances of digital mammography and DBT. They focused on women who participated in the TMIST Lead-in trial but were ineligible for the full trial due to their age at the time of study registration.
Final analysis included 271 women. Of this total, 181 were 40 to 44 years old, while the remaining 90 were aged 75 and older. For the younger age group, 105 women were randomly assigned to DBT while 76 underwent digital mammography. And for the older age group, 44 women underwent DBT while 46 were assigned to mammography.
Women in both study arms had 389 mammography exams and 482 DBT screening exams, respectively, making for an average of 3.2 screening rounds per woman in each arm. The researchers reported eight diagnosed cancers, with seven being screen-detected (6 by DBT, 1 by mammography). They also reported one interval cancer in the DBT arm.
DBT led to lower recall rates and higher cancer detection rates over mammography in the younger age group. In both age groups, DBT also improved the number of screening-related diagnosed cancers divided by the number of recalled exams (PPV1) and the number of screening-related diagnosed cancers divided by the number of screening-related biopsies performed (PPV3).
Comparison between DBT, mammography in TMIST Lead-in trial participants who are ineligible for full TMIST trial due to age | ||||
Measure | Age 40-44 | Age 75 and older | ||
| Mammography | DBT | Mammography | DBT |
Recall rate | 13.2% | 12% | 10.1% | 3.6% |
Cancer detection rate (per 1,000 exams) | 0 | 14.6 | 7.2 | 7.1 |
PPV1 | 0% | 12.2% | 7.1% | 20% |
PPV3 | 0% | 83.3% | 50% | 50% |
Seely said the study’s results correlate with other studies showing better screening performance with DBT over digital mammography.
“We are looking forward to the full TMIST trial in women aged 45 to 74 to confirm this in a much larger study, in women who are more likely to be screened,” she told AuntMinnie. “It [Lead-in study] found that using DBT, particularly in younger women, is likely beneficial.”
Seely noted that the Lead-in trial study was not tested for significance “due to its very small sample size and unplanned analysis.” She said the larger TMIST trial is expected to overcome the limitations of the smaller study.
Read the full study here.