FDG Positron Emission Tomography in the
Staging of Patients with Bronchogenic Carcinoma
General
Positron emission tomography (PET) relies upon actual physiologic information rather than morphologic features for the evaluation of bronchogenic carcinoma [74]. The most commonly used agent for PET tumor imaging is deoxy-glucose linked to 18-fluorine (a positron emitter). The agent 2-[F-18] fluoro-2-deoxy-D-glucose, or 18-FDG, competes with glucose for facilitated transport into cells and also competes with glucose for phosphorylation by hexokinase. Unlike glucose, however, the phosphorylated form is not further metabolized and remains in the cell [75]. The agent is useful for imaging bronchogenic carcinoma because lung tumor cells have an increased cellular uptake of glucose due to an increased number of surface transport proteins and a higher rate of glycolysis in comparison to non-neoplastic cells [17,76,77]. FDG PET imaging can have a significant impact on patient management by heightening suspicion for pulmonary malignancy, identifying unsuspected sites of disease, and by guiding selection of a biopsy site. Similarly, a negative PET scan indicates a low likelihood for malignancy and supports the use of conservative management and followup [136].
Increased glucose metabolism, however, is not completely specific for tumor [78] and can occur with infectious or inflammatory processes [79,132]. Similarly, lack of increased glucose metabolism does not necessarily exclude malignancy as carcinoid tumors [100] and bronchoalveolar cell carcinomas [101] may not demonstrate significant tracer uptake. Lesion detection on PET imaging depends primarily upon two factors: the amount of tumor uptake of 18-FDG and tumor size [80].
PET-FDG for Staging of Bronchogenic Carcinoma
Although PET-FDG imaging has been used in differentiating benign from malignant pulmonary nodules, this discussion will focus on the use of PET imaging in the staging of bronchogenic carcinoma. Imaging with FDG is done in the fasting state to minimize competitive inhibition of FDG uptake by glucose (elevated glucose levels can result in decreased FDG tumor accumulation) [138]. Imaging while fasting also minimizes cardiac activity and improves detection of mediastinal metastases [139].
Unlike conventional imaging, FDG PET has the ability to define both local and distant disease and is a powerful imaging tool that can have tremendous impact on patient management. Additionally, the combined use of CT and PET imaging may be cost effective for patient management [4]. A conservative strategy of using chest CT plus PET imaging has a potential cost savings of $1154 per patient [4,137]. This strategy would involve taking biopsy specimens from all positive findings with either CT or PET that might indicate non-resectable malignancy so that surgical candidates are identified more definitively [4,137]. The largest component of the cost savings realized by this approach results from prevention of unnecessary surgery in patients with unresectable disease [137]. Using this approach and assuming 85,000 patients (on the basis of national cancer statistics) undergo this diagnostic algorithm, the calculated savings would be $98,000,000 per year [139]. The discussion below will illustrate the role PET imaging plays in the TNM staging of non-small cell lung cancer.
Primary Tumor (T):
FDG PET imaging is of limited usefulness in determining the T status of the primary lesion [138]. Although tumor size can be estimated on PET imaging, this is best accomplished on CT scanning [137]. Additionally, PET scanning has limited accuracy in determining invasion into adjacent structures and for the detection of small satellite nodules [138,140]. One area in which FDG PET imaging is superior to CT scanning is in confirming a malignant effusion (T4 lesion) [131,154].The finding of increased FDG uptake greater than mediastinal blood pool activity that conforms to the pleural cavity is highly suggestive of a malignant effusion with an accuracy, of 80% to 92% [153,154]. The accuracy is slightly decreased as inflammatory or infectious pleural fluid collections can also demonstrate increased FDG accumulation [154].
Regional Lymph Node Metastases:
Conventional imaging:
Classification of lymph nodes on conventional CT imaging is based upon size. Mediastinal lymph nodes with a short axis diameter of greater than 1.0 cm are suspected of representing metastatic disease [152]. Unfortunately, up to 21% of nodes smaller than 1 cm are malignant and up to 40% of nodes larger than 1 cm are benign [152].
Exam interpretation:
Abnormal uptake in mediastinal or hilar nodes is typically defined as activity higher than the surrounding tissue uptake [141]. Standardized uptake ratios (SURs) have been evaluated to determine if there is improved detection of lymph node metastases. Quantification, however, poses a problem when determining activity on PET images in lymph nodes less than 1 cm in size because of the partial volume effects. This may falsely lower the SUR value [77] and visual assessment is generally as accurate as SUR determination [80].
Results:
Studies indicate that PET 18-FDG imaging is superior to computed tomography and magnetic resonance imaging in staging metastatic mediastinal lymph nodes in patients with bronchogenic carcinoma [124,133,141,152]. PET imaging can contribute complementary non-invasive functional information to the established size criteria for abnormal mediastinal lymph nodes which improves the overall accuracy of clinical staging for bronchogenic carcinoma [120]. Studies have shown that 18-FDG uptake within a normal sized node is highly suggestive of metastatic disease [17,76,78,80,81] and should be considered to represent malignancy until proven otherwise [146]. A number of PET studies have also demonstrated that the absence of 18-FDG uptake in enlarged nodes identified at CT is highly indicative of lack of metastatic involvement [17,78,81,82]. On a per patient basis, sensitivity for PET 18-FDG imaging in the detection of pathologic mediastinal lymph nodes has been reported to be between 67% to 92%, with a specificity between 97% to 100% (See table 2). Overall sensitivity is 83%, and overall specificity is 90%. Dwamena et al. performed a meta-analysis of 14 PET studies for staging mediastinal adenopathy and found an overall sensitivity of 79% (+/- 3%), and an overall specificity of 91% (+/- 2%) [124]. Accuracy was 92%, positive predictive value was 90%, and negative predictive value was 93% [124]. This is clearly superior to CT which has an overall reported sensitivity and specificity of 62% and 73%, respectively (using a transaxial short axis greater than 1.0 cm). PET staging of mediastinal nodes approaches mediastinoscopy which has reported sensitivities between 72% to 91% [141]. Results of the PET exam can be used to more accurately guide mediastinal exploration with improved yield from preoperative mediastinal lymph node sampling [151].
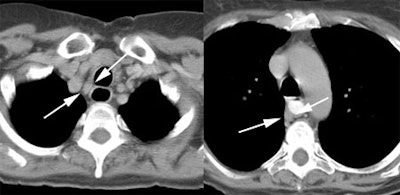
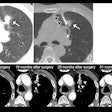
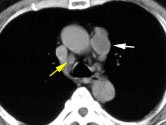
Example: This patient with a left lung non-small cell lung cancer demonstrated a pathologic aorto-pulmonary window node (N2) by CT size criteria (white arrow), and a non-pathologic retrocaval-pretracheal contralateral mediastinal node (N3) (yellow arrow). PET-FDG images revealed increased tracer accumulation within both nodes, consistent with metastases. Note the lack of anatomic resolution on the PET images. (Case courtesy of H. Page McAdams MD, Department of Radiology, Duke University Medical Center)
NOTE: To load a higher resolution view, simply click directly on any of the images below. |
||
 |
 |
 |
Limitations of FDG PET in lymph node staging:
Although PET 18-FDG imaging is clearly superior to helical CT for staging mediasitnal lymph nodes, it is not the "gold standard" for the confirmation or exclusion of N2/N3 disease in patients with NSCLC. False-negative examinations have been reported in association with both normal and enlarged lymph nodes that contained microscopic or small (under 5 mm) foci of tumor [17,76,79,80,129,133,140,142]. False-positive examinations have been reported in association with follicular hyperplasia [76,80,133], non-specific inflammation [81,83,129], epithelioid granulomas within nodes, pneumoconiosis [141], and anthracotic nodes [78,80,129,133]. Based upon these reports, a reduced specificity may be anticipated in populations with a higher incidence of granulomatous disease [141]. Reactive nodes in patients with post-obstructive pneumonitis may also be expected to produce false-positive exams. Uptake in a thyroid nodule can be misinterpreted as supraclavicular adenopathy [140].
PET studies interpreted without correlative anatomic imaging studies are less accurate, which reflects the general problem with PET studies -- they suffer from a lack of anatomic information [17,82]. Hilar nodes that are in close proximity to the mediastinum can be mistakenly classified as mediastinal nodes (false-positive interpretation)-- especially in the right tracheobronchial and subaortic region [17,133]. PET imaging can also be limited when the primary lesion is central. Distinction between uptake in the tumor and uptake in the adjacent hilar or mediastinal lymph nodes may not be possible without the use of CT correlation and even then the problem may not always resolved [17,80,82]. Increased sensitivity and accuracy have been demonstrated when PET image interpretation was combined with correlative CT images [17,82]. Combined interpretation or fusion images (which superimpose the physiologic PET data upon the anatomic CT images) probably best optimize the strengths of both imaging technologies [84,149]. Use of dual-modality PET/CT units further increases the number of patients correctly staged [152]. The accuracy for staging mediastinal lymph nodes increased from 89% with PET alone, to 93% with PET/CT (compared to 63% for CT imaging) [152]. The use of PET/CT can result in a change in the planned treatment in up to 15% of patients [152].
|
A central cancer near the aortopulmonary
window, as in this case, is difficult to separate from possible
mediastinal lymph nodes. |
|
|
Despite the fact that some authors advocate that patients with negative 18-FDG exams for pathologic mediastinal adenopathy should proceed to thoracotomy [74], such statements are premature. Although small, the number of false positives and false-negatives suggests that PET-FDG results should not supplant histologic confirmation for suspected mediastinal nodal metastases [82,133]. Surgical studies have demonstrated that patients with metastases detected at mediastinoscopy have a worse prognosis than patients in whom N2 disease is found only at surgery [15,18]. Prospective studies have not been performed to determine whether patients with negative pre-operative 18-FDG studies for mediastinal nodes have a prognosis similar to patients in whom N2 disease is found at thoracotomy following a negative mediastinoscopy.
Distant Metastatic Disease:
18-FDG PET has significant potential to be used for detecting extrathoracic metastases when whole body images are performed in conjunction with tomographic images of the chest [4,79,80,83,120]. Detection of unsuspected extra-thoracic spread can be identified in 6% to 24% of patients and can significantly alter patient management [80,106,120,133,140,141,143,144,151]. The likelihood for detecting unsuspected metastases increases in patients with locally advanced disease (ie: stage III), but 11% of patients with stage I or stage II disease on conventional imaging can be found to have metastases [144]. In another study, 13% of patients with T1 non-small cell lung cancer had extrathoracic metastases at the time of diagnosis, and another 11% developed extrathoacic metastases within one year [157].
|
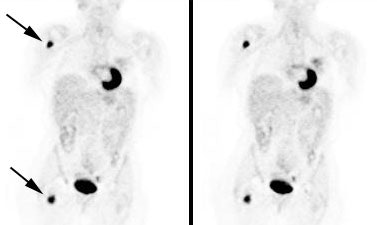
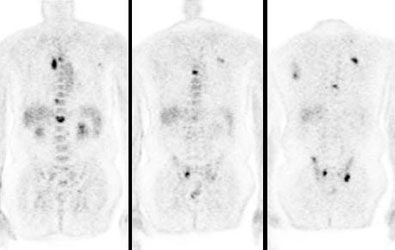
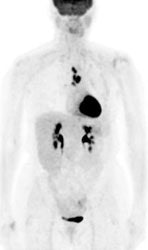
Unsuspected bone metastases: The patient shown below had a left lung non-small cell lung cancer (vaguely seen in the left lung on the PET images shown below). There was no uptake of tracer within the hila or mediastinum to suggest nodal metastases, however, unsuspected bone metastases were found in the right humerus and right hip (black arrows). These findings significantly altered patient management. |
|
|
|
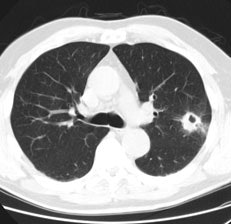
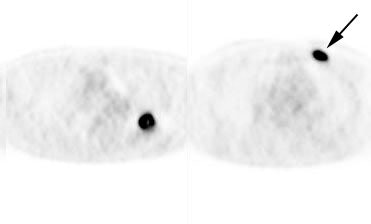
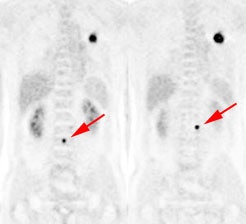
Unsuspected bone metastases: The patient shown below had a cavitary left lung non-small cell lung cancer. There was no uptake of tracer within the aortopulmonary window mediastinal nodes detected on CT to suggest metastases, however, unsuspected bone metastases were found in the left anterior 4th rib (black arrow- not detected on the patients CT scan) and lumbar spine (red arrows- not included in staging CT scan). The presence of bone metastases significantly alters patient prognosis and management. PET imaging provides a rapid whole body survey for the detection of unsuspected metastatic disease. |
|
|
Adrenal gland: PET imaging can also be used to exclude abnormalitiy in sites of suspected metastatic disease on conventional imaging [140]- especially for indeterminate adrenal lesions [120]. An exam is generally considered positive for malignancy if uptake within the adrenal lesion is greater than or equal to the liver [158]. FDG PET has been shown to have a sensitivity 93% to 100% for the characterization of metastatic adrenal lesions in patients with bronchogenic carcinoma (specificity 80-100% and accuracy 92-100%) [135,147,158]. If FDG uptake is normal in an adrenal mass in a patient with NSCLC, then patients should be considered for curative resection [135]. However, false negative exams can occur with necrotic or hemorrhagic metastases and with small lesions [158].
Adrenal adenomas can have uptake of FDG equal to or greater than the liver resulting in a false positive exam [147]. Generally, however, adenomas demonstrate only mild tracer accumulation that is less than liver activity, but greater than background [147].
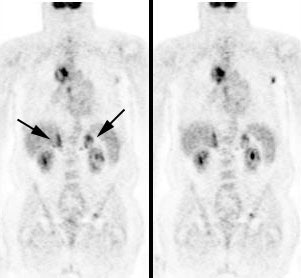
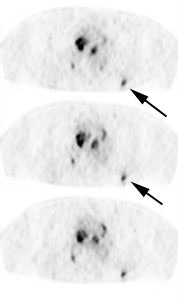
|
Bilateral adrenal metastases in a patient with non-small cell lung cancer: Uptake within the patients primary lung cancer can be seen within the right chest. Uptake within the bilateral adrenal glands (black arrows) confirmed the presence of adrenal metastases. |
|
|
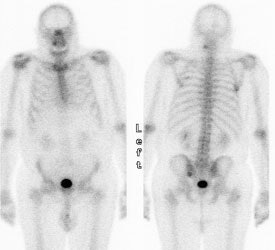
Skeletal metastases: FDG PET has been shown to be superior to bone scan for the detection of skeletal metastases- PET sensitivity 92%, bone scan sensitivity 50% [146].
|
Widely metastatic non-small cell lung cancer to bone: The bone scan (left) significantly underestimated the extent of skeletal metastases as demonstrated on FDG PET imaging (right) which revealed multiple vertebral body metastases. Click PET image to view cine of patients PET scan (1.4 MB) |
|
|
Malignant pleural effusion: PET FDG has also been shown to be abnormal in patients with malignant pleural effusions [131]. Increased pleural FDG uptake is highly suggestive of a malignant effusion (sensitivity 95%) [131].
CNS metastases: Although PET imaging is overall superior to conventional imaging for detection of metastatic disease, PET should not replace conventional imaging for evaluation of brain metastases [120,141]. The normal brain has substantial glucose uptake and metastatic foci may be difficult to detect on PET FDG images [120,141,146]. Urinary tract activity also limits evaluation of the genitourinary system [133].
False positive examinations for metastatic disease have been described [130,133,135,142,143]. As a result, a positive PET scan cannot be accepted as definitive proof of metastases and further staging procedures are usually required so that patients are not denied potentially curative surgery [130,133]. Of note, in one study a patient classified as having stage IV disease based upon the presence of a liver metastasis on PET imaging initially had a normal CT exam of the liver [130]. A follow-up CT exam revealed a metastatic lesion corresponding to the original PET abnormality [130]. This indicates that the initial CT was actually a false negative exam and that PET may be more sensitive than conventional modalities for detection of certain metastatic lesions [130].
Patient Staging/Management:
In the prospective evaluation of the utility of FDG PET for the primary clinical staging of patients presenting with non-small cell lung cancer, PET findings resulted in a different stage than the one arrived at by convention methods in 27% to 61% of patients [133,140,141,144]. Generally, FDG PET exam findings reveal more extensive disease than was suspected clinically- thereby reducing the likelihood of non-curative surgery in lung cancer patients [144,151]. This has a great impact on patient management decisions. FDG PET exam results can change or influence patient management decisions in 35% to 67% of patients [140,141,144]. A study by Seltzer et al. examined the impact PET exam results had on patient management by sending a questionnaire to physicians that had referred patients with known or suspected lung cancer for FDG imaging [150]. The FDG exam findings resulted in a change in patient stage in 44% of cases (29% upstaged, 15% down-staged) [150]. In this same study, the planned modality for treatment was changed in 39% of patients based upon the PET exam results [150]. In a prospective, randomized trial, FDG PET imaging has also been shown to decrease the number of futile thoracotomies (defined as surgery for a benign lesion, N2 nodal disease detected at mediastinal dissection, stage IIIB lesion, or death from any cause within one year) [151]. For patients with conventional workups (CWU), futile thoracotomy occurred in 41% of patients [151]. In patients that underwent CWU plus PET imaging, futile thoracotomy occurred in 21%- a 51% reduction from CWU alone [151].
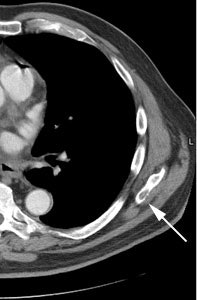
|
Change in stage: The patient below was felt to have Stage IIIB disease based upon the chest CT findings. FDG PET imaging confirmed ipsi- and contralateral mediastinal adenopathy, but also reveal a left scapular metastasis (seen retrospectively on the CT scan [white arrow]). A left iliac metastasis was also identified (black arrow right PET image). This resulted in a change in patient stage as the patient was now has Stage IV disease. |
|
|
van Titeren et al performed a randomized trial to compare conventional staging work up (CWU), to a staging workup that included FDG PET (CWU+PET) imaging. The study group included patients with suspected or proven non-small cell lung cancer. Patients were considered to have undergone a futile thoracotomy if the lung lesion proved to be benign, there was pathologically proven mediastinal lymph node involvement, or if the patient experienced recurrent disease or death from any cause within one year after randomisation. All potential sites of nodal or distant metastases which might have a major effect on patient management were confirmed by other means. Unconfirmed PET findings were ignored. Prior to surgery, PET imaging identified nearly twice as many patients (32 patients) with unresectable disease compared to CWU (18 patients). They found that a significantly greater number of patients in the CWU group (41%) underwent futile thoracotomy compared to the CWU+PET group (21%). Assessment of resectability by CT and PET was discordant in one-third of cases, and the PET exam was correct in two-thirds of these instances. PET imaging also helped guide preoperative mediastinal lymph node staging. The yield of preoperative node staging was 63% in the CWU group, compared with 83% in the CWU+PET group. Unsuspected distant metastases were identified in the CWU+PET group in 8% of patients. The addition of PET to conventional workup can strikingly reduce the number of futile thoracotomies in patients with suspected potentially resectable non-small cell lung cancer. It's main advantage is to upstage patients, alleviating unnecessary surgery and directing appropriate medical therapy.
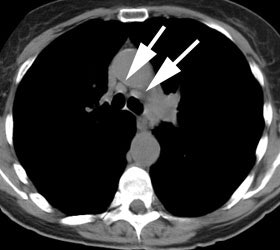
|
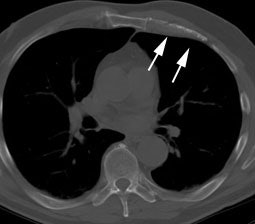
Futile thoracotomy- extensive mediastinal lymph node metastases: The patient below had a T1 lesion in the left lower lobe (black arrow). Pre-operative CT scan revealed lymph nodes within the mediastinum which were not pathologic by size criteria (white arrows). The patient underwent thoracotomy for tumor resection and was found to have positive hilar lymph nodes- a mediastinal node dissection was not performed. A post operative PET scan revealed extensive mediastinal lymph node metastases to the normal sized nodes. Had PET imaging been done pre-operatively, thoracotomy could have been avoided in this patient. |
|
|
However, PET findings should not be used in isolation without clinical, other imaging, or histologic data [142]. Up to 10% of patients classified as non-surgical candidates based upon FDG PET exam findings have been shown to have a lesser stage at surgery. Note however, that in this same study CT inaccurately classified 32% of patients as non-surgical [142] and PET has been shown to be substantially more accurate than CT in almost all comparative studies [144].
The spatial resolution of PET is generally insufficient to exclude small-volume disease [144] and FDG PET imaging can underestimate disease extent [142]. Up to 13% of patients classified as surgical candidates based upon their PET exam have been shown to have more advanced disease histologically (in this same study CT incorrectly classified 19% of patients with advanced disease as surgical candidates) [142].
In summary:
FDG PET imaging improves the overall accuracy of clinical staging for bronchogenic carcinoma through better identifications of nodal and distant metastases. In doing so, PET imaging has been shown to have a significant impact on patient management by better identifying those patients that will most benefit from primary surgical treatment. Similar to conventional imaging, PET suffers from both false-positive and false-negative exams. Additionally, PET imaging cannot replace the structural information provided by standard anatomic imaging techniques. Bronchial wall, pleural, and vascular invasion are difficult to image with PET and from a surgical perspective, an anatomical image remains necessary for operative planning [84]. Other limitations of PET imaging include its lack of widespread availability, the expense of the PET scanner itself, and the 110-minute half-life of the tracer, which necessitates that a cyclotron be available on site or close enough to allow timely FDG delivery [78]. FDG PET imaging is probably best viewed as a very useful complementary imaging modality to conventional methods for the clinical staging of patients with NSCLC.