Coal Miners Pneumoconiosis:
Clinical:
This disorder is due to coal dust inhalation and the inhaled carbon is the offending agent (not silica). The "coal macule" is the histologic lesion. Macrophages are not destroyed upon carbon ingestion, but the lesion develops due to back-up of the clearing mechanism. Many of these patients may have a mixed disease (ie: concurrent silicosis) due to heavy exposure to silica in coal mines. The disorder generally requires a period of at least 10 years exposure and it is radiographically indistinguishable from silicosis. The disease extent directly relates to the amount of exposure and the disease does not progress once exposure has been stopped. Many of these patients have a mixed disease, however, due to concurrent silica exposure. As with silicosis, the risk for tuberculosis is increased in patients with coal workers pneumoconiosis [2]. Types of disease include:
1- Simple form: Characterized by small nodular opacities with an upper lobe predominance, which less commonly calcify than in silicosis. Pulmonary function tests remain within normal limits and the disorder is arrested upon discontinuation of exposure.
2- Complicated form: Characterized by large opacities (>1cm) which are radiographically indistinguishable from the conglomerate masses of silicosis. This complicated form is also referred to as "progressive massive fibrosis" and emphysematous changes. FEV1, FVC, and diffusing capacity are all decreased.
3- Caplan's Syndrome: This syndrome is characterized by rheumatoid arthritis with pulmonary rheumatic nodules in coal workers. The nodules typically measure between 0.5 to 5 cm in size and may cavitate. Patients are rheumatoid factor (+). The nodules often develop concomitantly with joint disease, but they may precede the onset of arthritis by months or years.
X-ray:
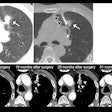
Computed tomography: On CXR, there are small round nodular opacities and occasionally reticular or reticulaonodular opacities [2]. The nodules are usually 1-5 mm in size and tend to be less well defined compared to those found in silicosis [2]. Calcification of the nodules is seen in 10-20% of patients on CXR- often as a central dot [2]. On CT, small nodules are seen diffusely throughout the lungs, but with an upper lung zone predominance [2]. Calcification of the nodules is found in 30% of patients [2]. Lymph node enlargement is seen in 30% of patients [2]. Egg-shell calcification is uncommon (only 1.3% of patients) [2]. In addition, centrilobular emphysematous changes are common in patients with CWP.
Progressive massive fibrosis with development of conglomerate masses is seen in complicated CWP [2].
REFERENCES:
(1) Radiol Clin North Am 1991 Sep;29(5):931-941
(2) Radiographics 2006; Chong S, et al. Pneumoconiosis: comparison of imaging and pathologic findings. 26: 59-77