Minnies winners, page 2
Best Radiologist Training Program
Winner: American College of Radiology Radiology Leadership Institute, Reston, VA
The Radiology Leadership Institute (RLI) is a relatively new arrival on the training and education scene, having been launched by the American College of Radiology in the summer of 2012. But RLI has already had a big impact, as evidenced by its selection as Best Radiologist Training Program by the Minnies panel.
 Dr. Cynthia Sherry. Image courtesy of ACR.
Dr. Cynthia Sherry. Image courtesy of ACR.That's a gratifying accomplishment to Dr. Cynthia Sherry, chief medical officer of RLI and chairman of the ACR Commission on Leadership and Practice Development. Sherry headed an ACR task force formed in 2010 that tackled the tricky topic of leadership in radiology -- more specifically, whether the specialty needed to step up its game, as traditional radiology practices were losing hospital contracts in the changing healthcare environment.
"RLI was hatched as an idea when not just radiology but medicine was at a crossroads," Sherry told AuntMinnie.com. "Reimbursement for radiologists was getting attacked from many corners, and there was one hurdle after another we had to get over."
Rather than produce another one-off meeting, the task force decided to pursue the creation of an ongoing program that would help train radiologists at all levels of their careers, not just the chosen few destined to become the head of a private practice or chair of a department. RLI participants can proceed through four different levels, each of which targets radiologists at a different stage of their careers, from residents on up. For the highest level, participants must complete a project designed to demonstrate what they have learned along the way.
"Some people are stimulated by milestones, and the levels are designed to cluster things in a way that encourages people to continue," Sherry said.
RLI offers a curriculum with a healthy dose of online learning to accommodate the busy schedules of radiologists who might not be able to take significant time away from their jobs or families. This is supplemented with annual events and meetings that bring participants together face to face. RLI attendees frequently can earn both CME and RLI credit at the same time.
There are seven broad areas of focus in the RLI curriculum: finance and economics; ethics and professionalism; legal and regulatory; strategic planning; practice management; professional development; and service quality and safety. There are also more than 150 of what Sherry calls "competencies," which participants can drill into across all seven domains.
RLI has also partnered with leading academic institutions outside of radiology, such as Babson College's Olin Graduate School of Business and the Kellogg School of Management at Northwestern University, which provided their management expertise to RLI activities.
There are currently just over 2,000 individuals enrolled in the RLI program, one-quarter of whom are young physicians, Sherry said. In February 2015, the group will hold RLI Expedition, a three-day event at the Omni Dallas Hotel that will offer scenario-based learning, with participants thrown into simulated crisis situations using actors to represent healthcare personnel.
How effective has RLI been in changing the terms of the debate in radiology? Sherry admits that RLI has struggled for ways to measure success, but one sure metric would be the number of radiologists who rise to positions of medical staff officer or hospital president. For her part, Sherry this month left private-practice radiology to take a job as chief medical officer at Texas Health Resources.
"Leadership is not something you are born into, it is something that you learn," Sherry said. "We believe you can't learn leadership simply by reading books, you have to get out there and do stuff."
Runner-up: Massachusetts General Hospital, Boston, MA
Best Radiologic Technologist Training Program
Winner: Thomas Jefferson University, Philadelphia, PA
For all the pain that new radiologists are experiencing in finding jobs, the market for radiologic technologists (RTs) may have suffered even more. The market is still struggling to right itself from the oversupply of radiologic science programs that popped up to address a shortage of RTs in the late 1990s. The Great Recession in 2008 didn't help things.
Through it all, Thomas Jefferson University has maintained its focus on training radiologic technologists with the flexibility and skills to survive in a rapidly changing job market. It does so by emphasizing credentialing and ensuring that when its graduates finish, they at least have a four-year college degree in hand, according to Frances Gilman, chair of the radiologic sciences department.
 The faculty at Thomas Jefferson University.
The faculty at Thomas Jefferson University.Gilman oversees a program that offers eight different imaging tracks, from radiography through MRI and CT to radiation therapy and medical dosimetry, with each program taking a year to complete. Applicants to the school must have a minimum of an associate degree, and they finish with a Bachelor of Science (BS).
Gilman believes that the focus on the BS degree fits well with the growing emphasis at many hospitals on quality. This often translates into a desire to hire staff members who are more credentialed and better educated.
"Hospitals are looking to employ practitioners with higher-level degrees," she told AuntMinnie.com. "The culture in radiology departments is changing a little bit, too, and I believe the focus is changing more to quality."
While trainees who graduate with a BS aren't necessarily making more money, they do have more flexibility, Gilman believes. Rather than exclusively focusing on one modality, she sees many Thomas Jefferson graduates working in radiography one day and MRI the next.
"It will open more doors for them," she said of the BS degree. "If they want to move into management or education, they have the degree. Our students do very well in the job market."
Runner-up: Weber State University, Ogden, UT
Most Significant News Event in Radiology
Winner: Evidence confirms slowdown in growth rate of medical imaging use
Many of radiology's recent woes can be traced to one immutable force: the U.S. government's drive to cut spending on healthcare in general and on advanced diagnostic imaging in particular.

This has led to round after round of Medicare reimbursement cuts, implemented in a variety of creative ways that only a federal bureaucrat would love. These range from direct changes to payment levels for specific procedures to alterations in the Byzantine formulas by which the government determines various aspects of reimbursement (just Google "CT code bundling" to learn more).
Whether by chance or by design, the reimbursement cuts appear to be slowly having an effect, reducing the sharp rate of growth in procedure volume that made radiology such a target in the first place. Over the past year, several studies have been published that demonstrate this phenomenon.
For example, in January, a study by market research firm IMV Medical Information Division indicated that after peaking in 2011, CT procedure volume fell by an average annual rate of 5.5% over the past two years. A few months later, a study by Thomas Jefferson University researchers, led by Dr. David C. Levin, came to a similar conclusion; they found that when Medicare bundled CT codes for the abdomen and pelvis in 2011, it led to a 29% drop in imaging payments for these procedures.
At the RSNA 2013 meeting, another study from Thomas Jefferson University declared that the era of rapid growth in advanced imaging is over. Code bundling led to sharp drops in utilization in the Medicare population in CT and nuclear medicine, particularly in 2010 and 2011, while use of MRI (which was never bundled) remained flat.
Is the decline in volume a good thing or a bad thing? Well, there's no denying that over the past decade it's been bad for radiology, with radiologist salaries remaining stagnant and the job market tightening up. But administrators at the U.S. Centers for Medicare and Medicaid Services (CMS) may have finally gotten the message, as new payment rates for 2015 announced in July largely spared diagnostic imaging from any major cuts. Radiology administrators even seem to be getting slightly more optimistic.
Things look even better if you have a longer horizon. In their RSNA 2013 presentation, Levin and colleagues noted that imaging procedure volume could be set for a long, gradual increase, due to the aging of the baby boomers and the addition of millions of uninsured individuals to the healthcare system under the Affordable Care Act.
Let's hope they're right.
Runner-up: Federal panel votes against Medicare coverage for CT lung cancer screening
Disclosure notice: AuntMinnie.com is a subsidiary of IMV Ltd.
Biggest Threat to Radiology
Winner: Commoditization of radiology services
As nice as it would be to blame all of radiology's woes on the U.S. government's Medicare reimbursement policies (see "Most Significant News Event in Radiology" above), that wouldn't really paint an accurate picture of what's going on in the specialty. Even as reimbursement drops, radiology is beset by market forces that are changing how business is done.

Much of this change is being driven by technology. Tools such as PACS make images available to everyone in a healthcare enterprise simultaneously, leading to radiologists holing up in reading rooms with less and less interaction with referring physicians.
Even more significant is the growing use of teleradiology. Once seen as a boon to radiologists by eliminating night call, teleradiology has become a bane by spurring the rise of a new cottage industry of teleradiology firms and national radiology providers that urge hospitals to eliminate the middleman (radiologists) by contracting directly with them.
The result? Traditional radiology practices are losing once-secure contracts with hospitals. Radiologists are being forced to compete on price rather than on quality or relationships, and new competitors are rising with radically different business models, such as second-opinion services marketed directly to patients that charge on a price-per-scan basis.
What's radiology to do? After years of ignoring the threat, the specialty finally seems to be taking the right steps, setting up new entities to train radiologists in the rough-and-tumble world of business leadership (see "Best Radiologist Training Program" above) and exhorting radiologists to get out from behind their PACS workstations to meet patients and referring physicians. Technology could even come to the rescue through tools such as Internet-based patient portals.
But most promising are efforts to radically restructure the way radiology is organized within the healthcare enterprise. Rather than physically isolate radiologists in their own department, what if they were distributed throughout the enterprise, embedded in clinical teams to provide consulting expertise directly at the point of care?
This vision isn't just a pipe dream -- it's due to be implemented at a hospital set to open in Qatar in 2015. And U.S. radiologists have experimented with the concept by embedding reading rooms in clinical areas.
Look for ideas like these to continue to percolate to the surface as radiology battles to make itself relevant again.
Runner-up: Decline in Medicare and third-party reimbursement rates
Hottest Clinical Procedure
Winner: Digital breast tomosynthesis
Digital breast tomosynthesis (DBT) continues its remarkable run in the Minnies, winning the award for Hottest Clinical Procedure for the fifth straight year, dating back to 2010.
The sustained interest in DBT is being driven by a steady stream of research papers on the technology's positive clinical impact, particularly on breast screening. Perhaps the most significant of these was a study published in June in the Journal of the American Medical Association, which found that adding tomosynthesis to mammography screening boosted cancer detection by 29% while reducing recalls by 15% (the study was named Scientific Paper of the Year by the Minnies expert panel).
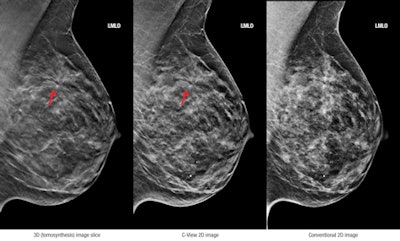 3D (tomosynthesis) image slice (left), C-View 2D image (center), and conventional 2D image (right). Images courtesy of Hologic.
3D (tomosynthesis) image slice (left), C-View 2D image (center), and conventional 2D image (right). Images courtesy of Hologic.Other recent papers have demonstrated that women in their 40s are most likely to benefit from screening with DBT (a finding that could shape the debate over breast screening in younger women), and that women with dense breasts are another population likely to benefit.
This year also saw the long-awaited arrival of a new entrant in the DBT market to challenge the Selenia Dimensions system from Hologic, as GE Healthcare received approval in August for its SenoClaire system. GE is highlighting the low radiation dose of the system and has already made the first U.S. installation. Next up is Siemens Healthcare, which in June announced that it had submitted a filing for its own DBT unit, Mammomat Inspiration.
Good news could also be on the horizon for DBT in terms of its financial return. Medicare currently doesn't pay any more for a DBT exam than it does for a conventional digital mammography study, even though DBT costs more. As a result, many women are paying out of pocket for the difference, although some private payors are reimbursing.
The U.S. Centers for Medicare and Medicaid Services (CMS) is said to be looking at adopting new CPT codes for DBT in the 2015 Medicare Physician Fee Schedule, perhaps as soon as November 1. Should that happen, digital breast tomosynthesis may remain radiology's Hottest Clinical Procedure for yet another year.
Runner-up: CT lung cancer screening
Previous page | 1 | 2 | 3 | Next page