The year ahead, page 2
CT lung cancer screening gets down to business
By Eric Barnes
2016 marks the first full year of reimbursement for CT lung cancer screening by the U.S. Centers for Medicare and Medicaid Services (CMS) -- and clinicians have plenty of work to do. New screening sites coming on board will join a CMS registry to enable the monitoring of results and radiation dose on a broad scale.
Researchers will be looking at how new algorithms for reporting and classifying findings, such as Lung-RADS, are performing. Are cancers being missed? Are too many subjects being referred for workup? Are patients returning for their second and third screening rounds? How can CT findings be used to fine-tune risk estimates and minimize the use of invasive workups?
In 2016, expect to see advocacy groups and clinicians push for screening to be expanded to groups beyond the somewhat conservative criteria used in the National Lung Screening Trial (NLST) -- criteria also adopted by CMS for Medicare payments. For example, CT lung screening could be cost-effective for individuals with a prior history of cancer, or those with fewer than 30 pack-years of smoking history.
Thus far, lung cancer screening has been concentrated on relatively well-off populations. Can the technology be diffused to include more individuals or different socioeconomic statuses? What are Medicare costs per patient or for successive annual screening rounds?
There's also the question of whether CT lung cancer screening will experience the same battle that has engulfed breast screening. The debate includes critics pointing to "harms" such as false positives, downstream tests, and patient anxiety as issues that must be weighed against the technology's proven mortality benefit.
In Europe, results from the first screening round of the Nederlands-Leuvens Longkanker Screenings Onderzoek (NELSON) lung cancer screening trial are expected in March. Will they suggest a mortality benefit approaching that of NLST? To date, most European trials have fallen far short of NLST's estimated 20% minimum mortality benefit from screening.
These issues and more will keep the CT lung cancer screening community busy in the year ahead.
Gadolinium concerns will loom over MRI
By Wayne Forrest
One major topic likely to receive continued attention in 2016 is the potential long-term health effects of gadolinium-based contrast agents (GBCAs).
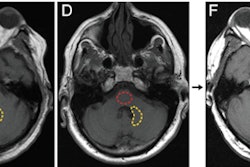
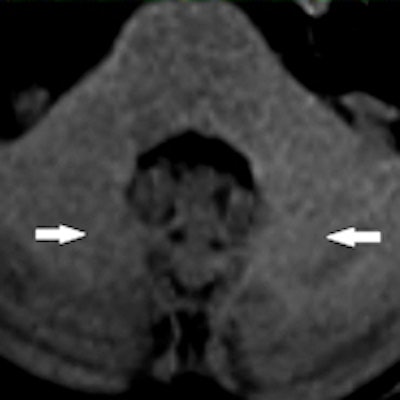
 Image courtesy of Kanda et al, May 5, 2015, and Radiology.
Image courtesy of Kanda et al, May 5, 2015, and Radiology.In 2015, evidence surfaced of lingering traces of gadolinium in the brains of patients who had received MRI contrast -- in some cases years after the scans occurred. Although it's still unclear whether the residual gadolinium is a safety risk, the news has prompted a review by the U.S. Food and Drug Administration (FDA) and the National Center for Toxicological Research (NCTR).
The agency plans to collaborate with researchers and vendors to learn how gadolinium could remain in the brain so long after administration. In the meantime, the FDA is asking healthcare professionals to consider limiting the use of gadolinium-based contrast to "clinical circumstances in which the additional information provided by the contrast is necessary."
The concern over gadolinium-based contrast has expanded into pediatric imaging, where two recent studies have explored potential aftereffects. In one study, researchers from Arizona found "quantitatively significant changes in signal intensity" in MRI brain scans of one pediatric patient who received 35 doses of a gadolinium contrast agent.
The good news is that gadolinium may not needed to enhance pediatric PET/MRI scans -- at least, according to a study from Stanford University. Researchers found "no significant difference in diagnostic accuracy" of MRI and PET/MRI for pediatric tumors regardless of whether gadolinium contrast was used.
What's next for nuclear medicine physician training?
By Wayne Forrest
The nuclear medicine community has been forced back to the drawing board after a plan to merge its physician training program into that of radiology was scuttled due to opposition from members.

"We are at a critical crossroads for our field," said Dr. Hossein Jadvar, PhD, president of the Society of Nuclear Medicine and Molecular Imaging (SNMMI), in the January 2016 issue of the Journal of Nuclear Medicine.
The crisis has been at a slow burn for years, but it reached the breaking point in 2015. The rise of hybrid imaging created an opportunity for radiologists trained in anatomical imaging to take over interpretation of PET/CT, SPECT/CT, PET/MRI, and other scans, as newly minted nuclear medicine physicians struggled with the studies.
A solution floated in 2015 by the American Board of Nuclear Medicine (ABNM) and the American Board of Radiology (ABR) would have merged nuclear medicine training with that of diagnostic radiologists and dissolved ABNM. But the proposal was shelved in the wake of opposition by SNMMI members.
To resolve the issue, SNMMI will form a task force early this year, and it has invited a number of nuclear medicine organizations to its 2016 Mid-Winter Meeting in January to brainstorm about the next course of action.
If and when support is achieved for a new plan, advocates will reach out to ABR, RSNA, the American College of Radiology, and other radiology stakeholders to gain a consensus on "comprehensive training of nuclear medicine practitioners, with opportunities for specialists from other disciplines, and ensure that nuclear medicine remains a vital, innovative component of quality care," Jadvar wrote.
Previous page | 1 | 2 | 3 | Next page