Minnies winners, page 2
Best Radiologist Training Program
Winner: American College of Radiology (ACR) Radiology Leadership Institute, Reston, VA
This year marks the second time in its relatively short four-year history that the Radiology Leadership Institute (RLI) has won the top award as the Best Radiologist Training Program.

Founded in 2012 by the American College of Radiology, the Radiology Leadership Institute has made strides in its mission to bring leadership training to radiologists at all levels of their careers. The ACR created RLI to help correct the growing chasm between the clinical training radiologists were receiving in medical school and the business and leadership skills that are becoming necessary in a healthcare environment increasingly driven by economics and public policy, according to Dr. Frank Lexa, chief medical officer (CMO) for RLI.
"We are developing programs for radiologists who need managerial skills who don't get that training in medical school," Lexa told AuntMinnie.com. "If you are a good radiologist and someone promotes you to be a section chief or join a leadership circle, all of a sudden you need help with reading financial statements."
Since becoming CMO of RLI a year ago, Lexa has focused on developing a flexible program that can be adapted to the career and educational needs of radiologists, rather than vice versa. The institute's content comes in a variety of formats, from online webinars to in-person destination meetings, such as the upcoming ACR-RBMA Practice Leaders Forum, being held January 13-15 in Orlando, FL, or its annual RLI Leadership Summit, being held September 7-10 at the campus of educational partner Babson College in Wellesley, MA.
Broadly speaking, RLI content is organized around the three stages of the average radiologist's career: finding a job, handling midcareer issues such as managing people and building business plans, and navigating later-stage issues such as helping top leaders like department chairs or CEOs achieve their full potential. Content can range from healthcare economics to regulation workforce trends and employment patterns.
So far, RLI has touched the career paths of 4,000 U.S. radiologists, and Lexa believes that the evolving format will help the group reach even more imaging professionals. To boost its reach, it also holds lunchtime meetings at the American Institute for Radiologic Pathology (AIRP), a four-week course in radiologic-pathologic correlation run by the ACR.
Ultimately, RLI's activities should improve radiology's position in a turbulent and changing healthcare environment.
"Our main goal is to help radiology with building better leaders," Lexa said. "That helps all of us in the house of radiology."
Runner-up: Duke University, Durham, NC
Best Radiologic Technologist Training Program
Winner: Johns Hopkins Hospital, Baltimore, MD
Johns Hopkins finds itself back on top as the Best Radiologic Technologist Training Program after last winning the category in 2013.

The program's sterling track record is due to the high quality of training that students receive, thanks to its affiliation with clinical care at Johns Hopkins, one of the pre-eminent medical institutions in the U.S. Students in the program's three main radiological sciences schools -- radiography, sonography, and nuclear medicine -- encounter a range of clinical conditions that they might not be exposed to at other programs, according to Sandra Moore, director of the Schools of Medical Imaging at Johns Hopkins.
"We are at Hopkins, where we do cutting-edge imaging," Moore told AuntMinnie.com. "Students get to see things and do things they may not see anywhere else."
It's a sentiment echoed by Dr. Karen Horton, interim chair of radiology at Johns Hopkins. The level of specialization among radiologists at the institution also filters down to technologists.
"The radiologists are superspecialized, and we have technologists who are superspecialized," Horton said. "That's how you go from good to great."
The Hopkins program is a bit unique in that most graduates go on to work within the Johns Hopkins system. At any given time, about 60 to 65 students are enrolled in the program, which requires an associate degree for entry. Once accepted, students participate full time in the program for 40 hours a week, and they can complete their training in 18 months. Johns Hopkins has agreements with local colleges for the prerequisite courses it requires for entry.
Moore believes that the job market for radiologic technologists is beginning to look brighter after a number of down years in which many graduates of radiological sciences schools had trouble finding jobs. Demand for technologists is growing, a trend she believes could be due to baby boomers finally beginning to leave the workforce after postponing retirement during the Great Recession.
Radiologic technology is a great career for anyone interested in healthcare, Moore said, but individuals must be dedicated to the work, rather than just seeking a comfortable job.
"You have to like working with sick people; don't just do it because it's a stable position," she said. "It's hard work, but if you love what you're doing that makes all the difference."
Runner-up: Weber State University, Ogden, UT
Most Significant News Event in Radiology
Winner: Rise of artificial intelligence and machine-learning systems
For most radiologists, artificial intelligence evokes a combination of both fear and hope -- deep-seated emotions that are perhaps the reason why this technology was named Most Significant News Event in Radiology by the Minnies expert panel.
The fear comes from the prospect that artificial intelligence and its technological handmaiden, machine learning, could one day become intelligent enough that they begin replacing radiologists in their primary mission of image interpretation. Some healthcare futurists are already predicting this development, such as Dr. Ezekiel Emanuel, PhD. In a controversial September 29 article in the New England Journal of Medicine, Emanuel wrote that machine learning will "displace much of the work of radiologists," and that this displacement would happen in "years rather than decades."
But others aren't so sure, and that's where the hope comes in. Artificial intelligence could become a huge boon to radiologists by freeing them from mundane tasks that few image specialists like to do, such as drawing measurements on 3D images or scrolling through vast stacks of screening mammograms.
Instead, artificial intelligence could lead to a gradual expansion of the role of radiologists in identifying disease and guiding treatment, as predicted by Dr. Bradley Erickson, PhD, in a webinar in August sponsored by the Society for Imaging Informatics in Medicine (SIIM).
Like Emanuel, Erickson believes that most diagnostic imaging will be performed by computers in 15 to 20 years, starting with simple studies and then moving on to more complex cases. But radiologists will still be needed to guide artificial intelligence, as well as interact with patients.
Until then, artificial intelligence marches on -- and is probably coming soon to an imaging facility near you.
Runner-up: American Board of Radiology to eliminate 10-year maintenance of certification exam
Biggest Threat to Radiology
Winner: Commoditization of radiology services
For the third straight year, the Minnies expert panel named the commoditization of radiology services as the Biggest Threat to Radiology.

The hat trick indicates there's been no letup in the confluence of forces leading radiologists to feel like their previously solid position in the healthcare landscape is beginning to shift under their feet. Teleradiology firms threaten them with disintermediation by contracting directly with hospitals, and the rise of national radiology groups undermines their historical independence as physician-entrepreneurs. Firms with radical new business models such as flat-price scans are even surfacing.
The changes indicate that radiologists are going to have to up their game if they want to stand out above the crowd. Social media offers one possible solution, giving imaging specialists the ability to come out of dark reading rooms and take more control over how they are perceived by the public, as indicated in a talk by Dr. Elliot Fishman at the 2015 International Symposium on Multidetector-Row CT.
Fishman believes that radiologists can use social media to facilitate communication with patients and also referring physicians, trainees, and other radiologists. This can help them set the terms of debate, not only about the appropriateness of different imaging tests (witness the ongoing controversy over screening mammography), but also the importance of radiologists in patient care.
Indeed, there are signs that patients actually prefer that radiologists interpret their studies, according to a study in the October issue of the American Journal of Roentgenology. What's more, researchers found a serious lack of understanding among patients about what radiologists do and what's involved in imaging exams.
Commoditization may be real -- but so are the solutions. Radiologists just need to get out there and prove their value.
Runner-up: Nurse practitioners reading medical imaging exams
Hottest Clinical Procedure
Winner: 3D printing of internal anatomical structures
As winner of the Hottest Clinical Procedure this year, 3D printing of internal anatomical structures has completed a seemingly overnight ascent to the top of the Minnies.
Once regarded as a curiosity, 3D printing is now being viewed as a revolutionary technology with a wealth of possibilities. Early applications range from printing structures such as orthopedic implants that can be customized for individual patients to creating models that can be used for education and surgical planning.
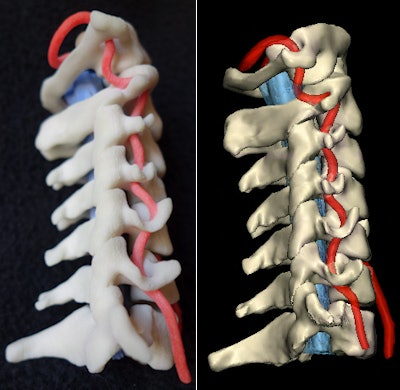 Physical 3D-printed model and virtual version. Image courtesy of Dr. Justin Cramer and Dr. Edward Quigley, PhD.
Physical 3D-printed model and virtual version. Image courtesy of Dr. Justin Cramer and Dr. Edward Quigley, PhD.A growing array of 3D printers and materials has given rise to products as diverse as titanium rib implants, ice skates for amputees, quality-control phantoms, soft-organ models for education, and surgical tools that can be printed at remote outposts where they could not easily be shipped. 3D-printed scaffolds can also be used to grow replacement tissues in the lab.
In the future, even functioning organs might be created by 3D printing. And because most medical applications of 3D printing are based on CT or MR images, radiology's role seems inseparable from the rapid evolution of the industry as a whole.
3D printing has even found applications in paleontology: An Australian group was able to create a 3D-printed reconstruction of the skull of a high-status woman from ancient Egypt, based on CT scans of her mummified body. The model was then used to create an amazingly lifelike face of the women, bringing the ancient world to life some 3,500 years later.
What's driving the rapid growth of 3D printing? Technological evolution is certainly a factor, as well as the growing need for spare parts in an aging population that is living longer every decade. For all the disappointing trends radiology has witnessed over the past decade, 3D printing represents an unambiguous win.
Runner-up: Digital breast tomosynthesis
Previous page | 1 | 2 | 3 | Next page