
Minnies winners, page 2
Best Radiologist Training Program
Minnies 2019 winner: Duke University, Durham, NC

The radiology residency program at Duke University sees its mission as training radiologists who excel at clinical work and patient care, according to Director Dr. Karen Johnson. While the program is very demanding, it produces residents who are ready for practically any clinical scenario by the time they graduate, she believes.
A novel aspect of the program is its 3/2 curriculum, the brainchild of former chair Dr. Carl Ravin some 20 years ago. Ravin foresaw the rise of subspecialized radiology and adapted Duke's residency program to emphasize subspecialization, with all residents guaranteed a fellowship.
Originally, the program offered three years of education in general diagnostic radiology and two years of fellowship training. Over time, that has evolved into the current curriculum, with the fourth year structured as a flexible year with up to 10 months of elective time.
Some residents use the flexible fourth year for research, while others participate in minifellowships, spending six months in a particular area that is distinct from their primary fellowship. The end result is that some residents have completed practically a dual fellowship by the time they graduate, Johnson said.
"I think of it as allowing residents to customize their training," she said. "It makes them exceedingly marketable in the workplace."
Another unique feature of Duke's program is that radiology residents are still taking autonomous resident call, bucking the trend at many academic programs for call to be taken over by attending physicians or outsourced to teleradiology firms. Johnson believes that Duke's ability to preserve autonomous resident call is a testament to the quality of the program's education, indicating that referring physicians are happy with the level of service residents are providing.
Duke has 13 residents in each class, with 10 focused on diagnostic radiology and three specializing in interventional radiology, said Johnson, who has been the program director since 2016. The chair of Duke's radiology department is Dr. Erik Paulson.
Johnson sees Duke's location as another major benefit. Unlike many academic centers, Duke is not located in an urban environment but in Durham, NC, a city of about 280,000 people. That means that, in addition to seeing complex cases from patients who fly in from around the world, they also encounter many of the conditions that are most likely to be seen with bread-and-butter radiology.
Johnson's advice to medical students who are interviewing with radiology programs? Be sure to talk to the residents.
"Residents won't hesitate to say what's good, what's not good, what could be better, and what's not working well," she said. "Applicants can see what's genuine and what's not."
Runner up: Emory University, Atlanta, GA
Best Radiologic Technologist Training Program
Minnies 2019 winner: Thomas Jefferson University, Philadelphia, PA
 Thomas Jefferson University.
Thomas Jefferson University.After a year hiatus, Thomas Jefferson University (TJU) has again won the award for Best Radiologic Technologist Training Program -- which Colleen Dempsey, EdD, the interim chair of the department of medical imaging and radiation sciences, attributes to the program's high levels of student and faculty commitment, administration and staff support, the variety of program offerings, and an emphasis on accreditation.
TJU offers a two-year baccalaureate degree for students who transfer with completed prerequisite courses. It also offers a one-year bachelor's degree for students who already have the prerequisite coursework and are medical imaging and radiation sciences professionals, a CT and PET/CT certificate program, and two master's degrees: one in medical imaging and radiation sciences and another in medical physics. The department offers undergraduate concentrations in radiography, CT, MRI, invasive cardiovascular technology, nuclear medicine, radiation therapy, medical dosimetry, general sonography, cardiac sonography, and vascular sonography.
And the university continues to add to its curriculum: Its most recent offering includes a women's imaging concentration. This new program will be available to students in fall 2020.
"We're constantly asking ourselves, 'What does the profession need, what do our students need, and how can we contribute?' " Dempsey told AuntMinnie.com.
Jefferson's commitment to accreditation is a point of pride, according to Dempsey. Not only is Jefferson regionally accredited, but the department boasts nine programmatically accredited programs from organizations including the Joint Review Committee on Education in Diagnostic Medical Sonography (JRC-DMS), the Joint Review Committee on Education in Radiologic Technology (JRCERT), the Joint Review Committee on Educational Programs in Nuclear Medicine Technology (JRCNMT), and the Commission on Accreditation of Medical Physics Education Programs, Dempsey said. And the quality translates into prepared graduates.
"Over the past two years, we've seen graduates begin new jobs within a month of graduation," she said. "They're getting full-time, well-paying jobs."
The program also seeks to serve its surrounding community, Dempsey noted.
"Our faculty and our administration are experts in their field -- top-notch professionals dedicated to educating our students," she said. "Offering high-quality programs is one way we can give back to our community."
Runner-up: Johns Hopkins University, Baltimore, MD
Most Significant News Event in Radiology
Minnies 2019 winner: Growth of artificial intelligence and machine learning in radiology

What more can be said about artificial intelligence (AI) in radiology? AI continues to be top of mind for the Minnies expert panel, such that it was voted the Most Significant News Event in Radiology for the fourth straight year.
While new clinical use cases for AI in radiology are still important topics, imaging specialists are beginning to look beyond such granular applications to examine AI and machine learning on a more holistic level. In particular, legal and ethical aspects of AI are generating a host of questions.
For example, would physicians face legal jeopardy if they render an incorrect diagnosis after following the recommendations of an AI algorithm? (Answer: Only if they don't follow existing standard of care). How can physicians influence the future direction of AI? (Answer: Only by embracing the technology). And will radiologists ever get paid for the use of AI? (Answer: Maybe, but they'll need to work for it).
Indeed, the ethical dilemma posed by AI is such that a call for an "AI code of ethics" was issued in October by seven North American and European radiology and imaging informatics organizations. The groups believe that the use of AI should be focused on helping patients and promoting the common good, rather than solely for financial gain.
The coalition calls for the creation of regulations, standards, and codes of conduct to be developed covering the use of AI in radiology, emphasizing transparency, patient protection, and version control of data and software. It evens calls for AI algorithms to be "properly vetted" before being put into use.
It's a great vision. But will it actually come to fruition? It's hard to say, but the thing about technologies like AI is, once they get out of the bottle, it's hard to put them back in.
Runner-up: Core Exam "fail" rate rises to highest level in seven years
Biggest Threat to Radiology
Minnies 2019 winner: Physician burnout

The selection by the Minnies expert panel of physician burnout as the Biggest Threat to Radiology is a stunning development that underscores the rapid rise of this important issue. In fact, "physician burnout" only first appeared in the list of Minnies radiology threats in 2018.
While burnout is affecting physicians across medical disciplines, it seems to be especially prevalent in radiology. Among the primary causes of burnout are a decline in physician autonomy, a growing number of nonclinical responsibilities, and a loss of work-life balance. Sound like any radiology department you know?
And burnout isn't just a professional issue. It's believed that burnout can contribute to economic losses and also a decline in the quality of patient care.
Burnout appears to be more prevalent at larger radiology practices compared with smaller groups, with one study finding burnout rates almost twice as high at larger practices. That's especially problematic given the consolidation trend sweeping radiology providers.
What can be done to alleviate physician burnout? They can start by dealing with burnout on a personal level, with individuals making sure they get enough exercise, eat well, and practice mindfulness, according to a talk by Dr. Cheri Canon of the University of Alabama at Birmingham at RSNA 2018.
But institutional changes also are important, she believes. Healthcare organizations must recognize that burnout is a real phenomenon and take steps to address it. What's more, administrators and department leaders should recognize that there's a human cost to focusing too much on goals such as shorter turnaround times and higher relative value unit (RVU) production.
Even little things can count, like not sending emails to staff in the middle of the night, or using financial incentives for improve performance, Canon believes. In the end, it seems that the solution to solving the problem of physician burnout starts at the top.
Runner-up: Corporate takeovers of independent radiology practices
Hottest Clinical Procedure
Minnies 2019 winner: 3D printing of internal anatomical structures
Interest continues to be high in 3D printing of internal anatomic structures, as evidenced by the technology being named Hottest Clinical Procedure by the Minnies expert panel for the third time in four years.
Researchers are finding that 3D models created from CT and MRI scans are great tools for applications like patient education and surgical planning. In particular, 3D models can be used to create implanted devices -- based on scans of a patient's anatomy -- that conform almost exactly to the body parts being replaced.
But 3D printing is also demonstrating its value as a research tool. For example, researchers from the U.S. National Institutes of Health used data from radiology's most powerful modality -- 7-tesla MRI -- to create 3D models of the brains of individuals with progressive multiple sclerosis. The models were then cut into slices for histological examination, which the researchers felt helped them understand the disease.
With respect to treatment planning, Australian researchers created 3D models from MRI and CT angiography scans that helped them simulate neurosurgical procedures. They felt the models were more accurate than conventional treatment planning techniques.
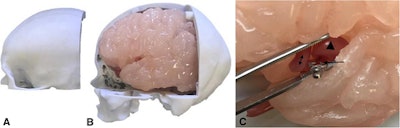 Patient-specific 3D-printed model for neurosurgery simulation, including a 3D-printed skull, brain, and artery with an aneurysm (arrowhead). Images courtesy of Nagassa et al and licensed under CC BY-NC 4.0.
Patient-specific 3D-printed model for neurosurgery simulation, including a 3D-printed skull, brain, and artery with an aneurysm (arrowhead). Images courtesy of Nagassa et al and licensed under CC BY-NC 4.0.Some hospitals may have been reluctant to take the plunge into 3D printing due to concerns over the cost of the technology. But those concerns were addressed by the release in July 2019 of current procedural terminology (CPT) codes that support insurance reimbursement for use of the technology. While the codes are currently temporary, radiology groups, including the RSNA and the American College of Radiology, are working to make them permanent.
Ultimately, the holy grail of 3D printing will be the creation of functioning organs. Indeed, researchers are already working on implants that can be printed from materials that mimic organ function, such as heart tissue.
It may sound like science fiction, but when you look at how far 3D printing has come in just a few years, it may not be that far off at all.
Runner-up: PET/MRI
Previous page | 1 | 2 | 3 | Next page



















