
Minnies finalists, page 2
Best Radiologist Training Program
The finalists for the Best Radiologist Training Program this year include two powerhouses in medical imaging, Emory University and Thomas Jefferson University.
Although both are well-regarded, neither program has captured top honors as Best Radiologist Training Program in the 22-year history of the Minnies.
Emory University, Atlanta, GA
Emory's roots in radiology began in the 1940s with the founding of its department of radiology, when x-rays were being used by medical professionals in the Atlanta community for basic imaging and therapeutic procedures.
Today, Emory's department of radiology and imaging sciences highlights the fact that it is one of the largest academic radiology departments in the U.S. Its diagnostic radiology residency program is headed by Dr. Christopher Ho, while Dr. Mark Mullins, PhD, serves as vice chair for education.
Emory prides itself on the diversity of its residents, as well as its status as one of the largest academic radiology departments in the U.S. This gives Emory residents access to a large number of patients and a wide breadth of cases, as well as access to the latest in medical imaging technology.
The department also touts its friendly atmosphere, which helps foster both hands-on learning and organized teaching. Emory maintains relationships with a number of community hospitals in addition to its flagship Emory University Hospital.
Thomas Jefferson University, Philadelphia, PA

Heralded as one of the top radiology residency programs in the U.S., Thomas Jefferson University's diagnostic radiology residency program trains radiologists in all aspects of medical imaging, with an emphasis on a friendly and stimulating learning environment.
The four-year program is continually updated to keep up with radiology's rapid advances, and the resident rotation schedule prioritizes the educational needs of the residents.
All clinical rotations are located on campus with the exception of pediatric radiology, as well as one rotation at the university's affiliated community-based hospital.
The program's curriculum also extends beyond traditional subspecialty radiology content to include topics such as business, imaging informatics, artificial intelligence, quality and safety, and health services research. It also boasts state-of-the-art technology.
Since the inception of the American Board of Radiology Core Exam, all graduating residents from the university have passed. While many residents pursue academic careers, the curriculum also prepares residents for careers in private practice.
Dr. Suzanne Long is director of the diagnostic radiology residency program, while Dr. Kristen McClure is assistant program director and director of residency selection.
Best Radiologic Sciences Program
The 2021 competition for Best Radiologic Sciences Program features two universities whose programs are familiar to the Minnies: Emory University and Johns Hopkins University. Both programs have won the category in previous years, Hopkins a stunning seven times, while Emory is the more recent victor in 2018. Which will triumph in 2021?
Emory University, Atlanta, GA
Emory trains tomorrow's radiologic technologists through its four-year Bachelor of Medical Science program, teaching students interpersonal skills in patient interaction.
Through a mix of classroom and clinical education, students learn and apply knowledge about anatomy, physiology, and pathology with patient positioning, radiation protection, and image acquisition techniques.
The degree program is available for participants with or without a current radiologic technologist credential. Advanced courses such as radiology administration, radiography education, and advanced clinical practice in CT and MRI are available. Students are challenged to learn effective oral and written communication skills, appropriate patient positioning, and radiation safety principles, as well as how to evaluate images and modify procedures for patients' needs.
Emory has a five-year average pass rate on the American Registry of Radiologic Technologists exam of 88.9% (first attempt within six months after graduation) and an average job placement rate of 100% (within 12 months of graduation). The program has been headed for the past four years by Ted Brzinski Jr.
Johns Hopkins University, Baltimore, MD
The Johns Hopkins Schools of Medical Imaging have multiple specialty education tracks for radiological technologists entering the field or making a midcareer change.
The program trains students in radiography, diagnostic sonography, or nuclear medicine, with training spanning 18 months for all three respective programs. All three programs boast a 100% employment rate within 12 months.
Johns Hopkins also offers advanced programs in CT and MRI that run five and six months, respectively, as well as a mammography training program that runs for three months.
The program emphasizes hands-on clinical experience along with theoretical training with the latest technology and expertise available to match the Johns Hopkins standards of excellence. Sandra Moore is director of the program.
For advanced training in MRI, CT, interventional radiology, or mammography, the university also offers on-the-job training programs. Students obtain firsthand clinical experience at Johns Hopkins' affiliated facilities, as well as other clinical facilities throughout the Baltimore-Washington, DC, metropolitan region.
Most Significant News Event in Radiology
Named Most Significant News Event in Radiology in 2020, the COVID-19 pandemic continues to cast a large shadow over radiology, as with the rest of the world. So it's no surprise that the pandemic is also a finalist in this year's competition.
But COVID-19 wasn't the only news story in radiology this past year. 2021 also saw a final recommendation by the U.S. Preventive Services Task Force on its guidelines for CT lung cancer screening that lowered the starting age from 55 to 50.
COVID-19 pandemic and its impact on radiology

It's no surprise the Minnies expert panel again picked the COVID-19 pandemic as a finalist for the Most Significant News Event in Radiology. Consider that last year at this time, vaccines weren't yet part of the arsenal.
Findings by radiology modalities prompted warnings -- first anecdotally and then in larger studies -- that COVID-19 vaccines can manifest on imaging in ways that mimic disease. Particularly confounding was that abnormal PET radiotracer uptake appeared to mimic malignant cancer.
As anecdotal reports of loss of smell and other neurological effects of COVID-19 infection began rolling in, so did reports aiming to shine a light on how the SARS-CoV-2 virus affects the brain and the mechanisms involved.
MRI proved to be an effective way to track COVID-19's lasting neurological effects in so-called "long COVID" patients, with neurological and neuropsychological sequelae reported in up to 30% to 40% of COVID-19 survivors.
The pandemic dominated topics at major meetings, virtually all of which were held online. At the Society of Nuclear Medicine and Molecular Imaging event, the 2021 Image of the Year went to a study that showed COVID-19 long-term neurological changes are associated with cognitive impairment.
The COVID-19 pandemic wrought seismic changes on the field of radiology, but there were bright spots.
The pandemic didn't seem to make a big dent in salaries for radiology professionals in 2020 and radiology personnel may be weathering COVID-19-induced stress and anxiety better than their colleagues in other parts of the hospital.
Just one and a half years into the worst healthcare crisis in 100 years, radiology has answered some but posed many more questions that need to be addressed about COVID-19 moving forward.
Medicare proposes revisions to payment criteria for CT lung cancer screening
In March, the U.S. Preventive Services Task Force (USPSTF) released an updated, final recommendation for CT lung cancer screening that lowered the starting age from 55 to 50 and adjusted smoking history from 30 pack years to 20 pack years. The guidance updated the task force's 2013 recommendation.
In brief, the recommendation now states that adults between the ages of 50 and 80 who have a 20 pack-year smoking history and currently smoke or have quit within the past 15 years should undergo annual screening for lung cancer with low-dose CT.
As in 2013, the task force has given the guidance a "B" grade, which translates to the following:
"The USPSTF concludes with moderate certainty that annual screening for lung cancer with low dose CT has moderate net benefit in persons at high risk of lung cancer based on age, total cumulative exposure to tobacco smoke, and years since quitting smoking," the group wrote.
Ultimately, the USPSTF noted the adjusted guideline should help catch lung cancer earlier, when it is more treatable, and also mitigate healthcare inequities, particularly differences among racial/ethnic groups and between men and women.
Biggest Threat to Radiology
Burnout of physicians

It's telling that in a year in which the COVID-19 pandemic continued to wreak havoc on radiology operations, burnout of physicians still emerged as one of the two biggest threats to radiology, as judged by the Minnies expert panel.
But when you think about it, perhaps it's no surprise. Well into the second year of the pandemic, burnout among front-line healthcare professionals has become more the norm than the exception. And while radiologists aren't exactly on the front lines of medical care, they play an important supporting role and can experience the same stresses.
A report from the U.K. chronicled how the COVID-19 pandemic caused stress among radiology staff like radiologic technologists. One of the major stressors was dealing with the need to reconfigure equipment and workflow in an era of heightened infection control.
Unfortunately, the pandemic has hindered the ability of radiology departments to adopt wellness strategies to counteract the rising feeling of burnout. Remote work and social distancing can make radiologists feel more isolated and less connected, according to some experts.
Ironically, at least one study released during 2021 posited that radiology personnel might actually be set up to better weather COVID-caused burnout. Researchers from Singapore found that -- at least at their institution -- high levels of job satisfaction in the radiology department and fewer instances of longer work shifts were protective against burnout.
Decline in Medicare and third-party reimbursement rates

This threat to radiology is an old bugaboo that was named the Biggest Threat to Radiology five times from 2007 to 2013, but it hasn't appeared at the top of this Minnies category since then. What a difference a few years makes.
The U.S. government seems to once again be taking aim at payments for imaging services in its Medicare and Medicaid programs, and the instrument of its wrath -- the U.S. Centers for Medicare and Medicaid Services (CMS) -- has proposed additional cuts for 2022.
For example, CMS has proposed what amounts to a 4% cut in payments to radiologists in its Medicare Physician Fee Schedule -- but even that's not as bad as the 10% that was originally proposed. And proponents of radiology are urging CMS to delay these cuts, so stay tuned.
More significantly, CMS has proposed a major change to radiation oncology reimbursement that would see Medicare move from paying for treatments in individual sessions to bundling payments into a single episode of care. The radiation oncology community is contesting this proposal, however.
On the positive side, CMS has once again kicked the can down the road when it comes to implementing the penalty phase of its appropriate use criteria (AUC), which requires that referring physicians use clinical decision support when requesting imaging studies.
Hottest Clinical Procedure
This year's finalists for Hottest Clinical Procedure are two modalities that are relatively new in medical imaging, 7-tesla MRI and photon-counting CT. In fact, neither has ever won the category.
7-tesla MRI
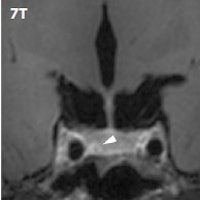 7-tesla MRI showing pituitary lesions. Image courtesy of Dr. Jeroen Hendrikse.
7-tesla MRI showing pituitary lesions. Image courtesy of Dr. Jeroen Hendrikse.Once thought to be relegated to research labs, 7-tesla MRI is beginning to be used as a clinical tool for some applications. In particular, the ultrahigh-field modality seems to be particularly well-suited to brain applications.
7-tesla MRI can produce contrast-to-noise ratios and anatomical detail that can give clinicians the confidence to diagnose subtle pathologies like microbleeds and infarcts in the brain. Even intracranial atherosclerosis is visible, according to a 2019 presentation on the technology at the European Congress of Radiology.
But 7-tesla MRI can also be useful outside the brain. Both vascular and parenchymal lesions are more visible with the technique, and the extremely high resolution of the modality is also useful in sports imaging for visualizing musculoskeletal problems like meniscus tears and other types of pathology. A talk on 7-tesla MRI for sports imaging was presented at the International Society for Magnetic Resonance in Medicine (ISMRM) meeting in May.
But there are downsides to 7-tesla MRI. The most obvious are the costs involved in acquiring, siting, and operating such massive scanners, as well as the additional challenges in preserving the safety of patients and staff in the presence of stronger magnetic fields. What's more, clinicians need to be aware that 7-tesla MRI could lead to more false-positive results, leading one expert to suggest its use only in high-risk patients.
Having said that, 7-tesla MRI looks set to continue to make inroads in clinical practice, especially as at least two vendors have 510(k) clearance to market their ultrahigh-field magnets for clinical use. Regardless of how it finishes in the 2021 Minnies, expect more great things from 7-tesla MRI in the years to come.
Photon-counting CT
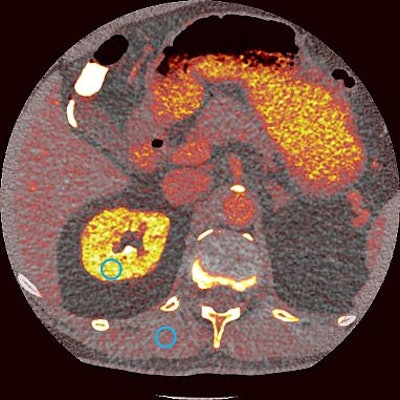 Photon-counting CT scan. Image courtesy of the U.S. National Institutes of Health.
Photon-counting CT scan. Image courtesy of the U.S. National Institutes of Health.Photon-counting CT is another medical imaging technology that's slowly making the move from the research lab to the bedside. The technology offers the potential to give radiologists much more detailed images at a lower radiation dose than conventional CT.
Photon-counting CT scanners are based on special detectors that count the number of incoming photons and measure photon energy. This can produce images that -- like 7-tesla MRI -- have a higher contrast-to-noise ratio, resulting in higher resolution and the correction of artifacts like beam hardening.
One of the first photon-counting CT scanners in the U.S. went into use at the Mayo Clinic in 2014. Researchers using that system found that it was able to cut radiation dose by 80% while matching the image quality of traditional CT for imaging of the sinus and temporal bone.
In April 2021, Mayo researchers acquired the first cardiac image on a new version of their photon-counting technology, and they compared the technology to other milestone achievements in CT like spiral scanning, multidetector-row imaging, and dual-energy CT.
And the major imaging OEMs are starting to show interest in photon-counting CT -- just as they are with 7-tesla MRI. In just the last year, at least two OEMs have acquired photon-counting detector developers, perhaps giving them a leg up on the next generation of CT technology.
Previous page | 1 | 2 | 3 | Next page



















