Minnies winners, page 2
Best Radiologist Training Program
Minnies 2021 winner: Emory University, Atlanta, GA
Emory is a powerhouse in medical imaging, winning Minnies awards in various categories since 2000. This year though is the first time the university has won the Minnies award for Best Radiology Training Program. However, program director Dr. Christopher Ho said the university's pedagogical approach has remained the same.
"There's a whole team of us here and everyone is so committed to the educational programs that it's just nice to see the recognition for it," said Ho, who has been leading the program since 2015. "We're a pretty low-key program, but the focus for us is really the hands-on approach for the residents. It's a really high-volume practice."
Emory's department of radiology and imaging sciences is one of the largest academic radiology departments in the U.S. Its four-year residency program usually has 18 residents a year who receive hands-on learning with the latest technology in a wide breadth of cases. The goal is for the residents to be career-ready radiologists upon completing the program.
Through the hands-on learning approach, residents are challenged with real-world tasks such as making the right decisions, helping manage patients, and supporting referring physicians. In addition to its flagship Emory University Hospital, the university also maintains relationships with various community hospitals in the greater Atlanta area and beyond.
The training program boasts a 100% rate for residency completion and employment with about 25% of residents going into academic-related jobs. Furthermore, "Most of our residents tend to do subspecialty work in future practices," he added.
While 95% of residents have returned to in-person training, some aspects of virtual learning that were used widely during the early days of the COVID-19 pandemic are still in use, according to Ho.
As for Ho, the marriage of being a consultant to physicians and helping patients through critical issues, as well as combining technology with patient care, are what drew him to radiology in 2003 during his fourth year of medical school. Prior to that, he believed his career would be in pediatrics.
Today, along with his position at Emory, Ho is a board-certified radiologist who specializes in breast imaging and breast interventions. He is also a manuscript reviewer for the journals Academic Radiology, Cancer, and Radiographics.
Ho said the hands-on learning he received while in medical school for his bachelor's and doctorate degrees translates to what Emory residents today learn.
"I want the residents to be independent from the beginning so they can formulate their own ideas. I don't want them to be scribes and tell them what to say," he said. "There's something to be learned from the cases they receive."
Ho credits support from Emory's administration, leadership, and education teams for the program's success.
Runner-up: Thomas Jefferson University, Philadelphia, PA
Best Radiologic Sciences Training Program
Minnies 2021 winner: Johns Hopkins University, Baltimore, MD
Johns Hopkins University is world-renowned for its health sciences programs that boast the latest technology for students to use. But as the university receives its record eighth Minnies award in this category, Sandra Moore, director of the schools of medical imaging, says there's more to the school than just the name.
"We're on the cutting edge of technology and the students get a great amount of clinical time so when they graduate, they hit the ground running and are ready to go," said Moore, who previously directed the radiography program at Johns Hopkins Hospital for 18 years. "We make sure they take advantage of that. And our faculty and staff are deeply committed to the success of students."
Moore knows from experience -- she graduated from the university's imaging program in 1994 with a certificate in radiography after a career as a school teacher. She later obtained her certification in mammography.
The program trains students in radiography, diagnostic sonography, or nuclear medicine over the span of 18 months for all three respective programs. All three programs boast a 100% employment rate within 12 months.
Johns Hopkins also offers advanced programs in CT and MRI that run five and six months, respectively, as well as a mammography training program that lasts for three months.
The cutting-edge technology, clinical rotations for students, and administrative support help with the program's emphasis on hands-on experience and theoretical training, which creates an environment for students who are either entering the field or making a midcareer change. Moore said the expertise available from the program's faculty and staff matches the Johns Hopkins standards of excellence for students to be ready for their career tracks as soon as they graduate.
"Once they graduate, they're ready for just about anything," Moore told AuntMinnie.com. "They've worked on different equipment, with different physicians and technologists, and with multiple protocols."
The university also offers on-the-job training programs for advanced modalities like MRI, CT, interventional radiology, and mammography. Students obtain firsthand clinical experience at facilities affiliated with the Johns Hopkins system, as well as other clinical facilities throughout the Baltimore/Washington, DC, metropolitan region.
"I always tell my students they should never be bored because there's always something different to do in this field," Moore said.
However, it's not just the students who learn; radiology physicians and technologists who help teach courses within the programs are also constantly learning. Moore herself goes by a quote attributed to the artist Michelangelo: "Ancora imparo," which translates to "Yet, I am learning." For Johns Hopkins, this applies to faculty as they are encouraged to pass on what they've learned to students.
"It's remarkable what you can do in this field. It's a testament to our field in the imaging sciences that there are so many ways you can go," Moore said. "When you come from Johns Hopkins, you're expected to be among the best. That reputation will stay with you."
Runner-up: Emory University, Atlanta, GA
Most Significant News Event in Radiology
Minnies 2021 winner: COVID-19 pandemic and its impact on radiology
For a second year, the Minnies expert panel picked the COVID-19 pandemic as the Most Significant News Event in Radiology.
News headlines in 2021 reflected radiology's pivot from reacting to the crisis to helping manage it, especially in reporting effects of the SARS-CoV-2 virus in infected people and patient responses to the vaccines. Also, there were significant reports -- several optimistic -- on the COVID-19 pandemic's impact on radiology.

As anecdotal reports of loss of smell and other neurological effects of COVID-19 infection began rolling in, so did reports aiming to shine a light on SARS-CoV's impact on the brain and the mechanisms involved.
MRI proved itself to be an effective way to track COVID-19's lasting neurological effects in so-called "long-COVID" patients, with neurological and neuropsychological sequelae reported in up to 30% to 40% of COVID-19 survivors. In another study using MRI, U.S. National Institutes of Health (NIH) researchers found brain damage in some patients who died of COVID-19 yet showed no signs of SARS-CoV-2 in tissue samples. Also, x-ray, CT, ultrasound, and MRI can all play an important role in the diagnosis and evaluation of COVID-19-related musculoskeletal pathology.
The pandemic dominated topics at major meetings, almost all of which were held online. At the Society of Nuclear Medicine and Molecular Imaging (SNMMI) event, the 2021 Image of the Year went to a study that showed COVID-19 long-term neurological changes are associated with cognitive impairment.
As COVID-19 vaccines began rolling out, early findings by researchers using a variety of modalities -- anecdotally and then in larger studies -- prompted warnings that vaccines can manifest on imaging in ways that mimic disease. Mammography, ultrasound, PET, and hybrid imaging all reported the manifestation, primarily showing lymph node uptake after patients received vaccines. Particularly confounding was that abnormal PET radiotracer uptake appeared to mimic malignant cancer.
Questions arose on whether the messenger RNA (mRNA) COVID-19 vaccines cause myocarditis with an MRI study suggesting that indeed may be the case and several sad events highlighted the potential risks of the vaccines. In January, a radiologic technologist died in Southern California after receiving the second dose.
Also, artificial intelligence (AI) models appeared to come into their own, especially in x-ray as researchers responded with one study after another offering algorithms for use in triaging COVID-19 patients, particularly in underserved populations worldwide. Whether these models will be put to use remains to be seen with many efforts now focused on how to best implement them.
As with the rest of society, the COVID-19 pandemic wrought seismic changes on the field, but there were bright spots. The pandemic didn't seem to make a big dent in salaries for radiology professionals in 2020, according to SalaryScan, AuntMinnie.com's annual survey of benefits and compensation in radiology.
And radiology personnel may be weathering COVID-19-induced stress and anxiety better than their colleagues in other parts of the hospital. In fact, high levels of job dedication and fewer instances of longer working shifts appear to be protecting radiology staff from anxiety and burnout.
Outpatient imaging volume slowly recovered. Growth in PET, CT, ultrasound, and MRI exam volume from June 2020 to June 2021 all exceeded a 15% increase in total hospital activity nationwide, according to a report from Syntellis Performance Solutions. The decline in imaging still appears greater than its recovery, however.
Importantly, socioeconomic issues have come to the forefront. The COVID-19 pandemic has negatively affected racial and ethnic minority populations and highlighted persistent historical disparities in healthcare. Radiologists were called upon and appear ready to help reduce disparities around COVID-19.
Just 1.5 years into the worst healthcare crisis in 100 years, radiology has answered some -- but posed many more -- questions that need to be addressed about COVID-19 moving forward. That is perhaps the most significant reason the COVID-19 pandemic wins the Most Significant News Event in Radiology category in the Minnies.
Runner-up: Medicare proposes revisions to payment criteria for CT lung cancer screening
Biggest Threat to Radiology
Minnies 2021 winner: Physician burnout
The COVID-19 pandemic has focused a spotlight on physician burnout, which was already becoming a serious issue across healthcare. As the pandemic grinds on, it seems like burnout is a problem that's only going to get worse.

Most definitions of burnout classify it as a prolonged feeling of work-related stress that can lead to lack of motivation and exhaustion. In 2011, about half of radiologists reported feeling burned out, a number that rose to 60% by 2014. A more recent survey in 2020 found that as many as 78% of respondents were "highly burned out" by at least one measure.
What's driving burnout in radiology? The data deluge is certainly one culprit, with radiologists increasingly swamped by a rising cascade of image data being produced by increasingly powerful modality scanners.
The nature of the work that radiologists do has also fundamentally changed -- also due to technology. Radiologists were once known as the "doctor's doctor," and imaging specialists reveled in the consultative role they played in working through challenging cases with referring physicians.
That all changed with the arrival of PACS, which moved image interpretation from consultations around a lightbox to radiologists ensconced in front of workstations in darkened reading rooms (not necessarily in the hospital basement, but sometimes it felt like it).
So what can be done about burnout? Admonitions to physicians to "heal thyself" through self-care and other small personal actions ring hollow when the problem appears to be so systemic and intractable. However, some facilities are beginning to take action, such as an acute care center that replaced 24-hour call with 12-hour shifts instead.
Some key opinion leaders in radiology believe that another solution could come from technology, specifically artificial intelligence (AI). Multiple deep-learning algorithms are being developed to take over tasks thought to be burdensome to radiologists -- and not just interpreting routine studies.
For example, one of the winners of this year's Minnies award for Best New Radiology Vendor is a company that's developed an algorithm designed to save radiologists an hour a day by generating the "impressions" section of radiology reports. Other companies are developing similarly creative applications.
Whether a technology-based approach to relieving burnout among radiologists works remains to be seen. But many of the specialty's brightest minds are giving it a shot.
Runner-up: Decline in Medicare and third-party reimbursement rates
Hottest Clinical Procedure
Minnies 2021 winner: Photon-counting CT
For years, photon-counting CT has been a technology that's tantalizing, but still just on the horizon. It now seems that photon-counting CT has finally arrived.
What caused the change? On September 30, the U.S. Food and Drug Administration (FDA) announced it had cleared the first photon-counting CT scanner for commercial marketing (Naeotom Alpha from Siemens Healthineers). In announcing the clearance, the FDA said the scanner was the "first major imaging device advancement" in CT in nearly a decade -- heady words from an agency that's notoriously conservative.
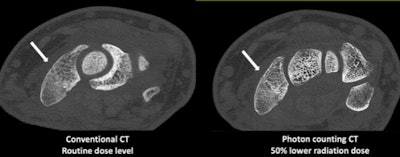
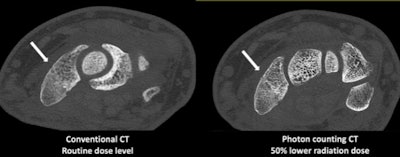 Conventional and photon-counting CT scans of the same patient demonstrate improved visualization of trabeculae and a wrist fracture while using 50% less radiation. Images courtesy of the Mayo Clinic.
Conventional and photon-counting CT scans of the same patient demonstrate improved visualization of trabeculae and a wrist fracture while using 50% less radiation. Images courtesy of the Mayo Clinic.So what's the fuss all about? To understand photon-counting CT, it's useful to first take a step back and look at the technology behind traditional CT detector design. CT images are created by converting x-rays that hit a solid-state CT detector into light; this light is then converted into electrical signals that can be read by a computer and reconstructed into images.
But this is a two-step process that can be inefficient, according to Cynthia McCollough, PhD, of the Mayo Clinic. Since 2014, McCollough has been part of a Mayo team working with Siemens on photon-counting CT and they began using the Naeotom Alpha system earlier this year.
Instead of the two-step process with light conversion, photon-counting CT counts individual x-ray photons as they strike the detector. This provides far more detail about the origin and type of photons, such as whether they are high energy or low energy.
McCollough likens photon-counting CT to water filling a bucket. With conventional CT, there was no way to differentiate whether water filled the bucket drip by drip or in an entire gallon poured in at once. With photon-counting CT, that's now possible.
It has taken decades of work to be able to mass produce the semiconductor material used to perform the one-step detection process. Also, to count individual photons, detector elecronics must be very fast. This explains why it's taken so long for photon-counting CT to become a clinical reality. But now that it is, McCollough is excited about its prospects.
At Mayo, researchers have now performed over 800 scans since 2015 on patients using various iterations of photon-counting CT technology. McCollough sees the technology as being particularly valuable in measuring low-energy x-ray photons, which with conventional CT instrumentation are typically "drowned out" by high-energy photons.
How does this translate into clinical utility? Photon-counting CT can be well-suited to visualizing iodine, which can lead to higher contrast-to-noise ratios and as a result, less contrast media can be used. Scans can also be performed at a lower radiation dose, McCollough said.
On the other hand, radiation and contrast dose can be maintained at the same level as conventional CT, leading to improved visualization of subtle pathology, as well as improvements in lung, musculoskeletal, and vascular images. Even bread-and-butter CT exams like abdominal studies will benefit, she said.
In fact, word is starting to get out among Mayo's referring physicians about the technology as a new tool to help them manage their patients.
"Doctors are starting to ask for the photon-counting scanner," McCollough said.
Like the FDA, McCollough is bullish on the future of photon-counting CT. As with spiral scanning and multidetector-row CT, she sees photon counting as eventually becoming mainstream, moving from the super-premium tier to eventually all the segments of CT.
"I think it is the future," McCollough said. "Ten years from now, all new systems will come with this."
Runner-up: 7-tesla MRI
Previous page | 1 | 2 | 3 | Next page