Minnies finalists, page 2
Best Radiologist Training Program
This year's competition for Best Radiologist Training Program features two well-respected radiology residency programs that have had great success over the years in training aspiring radiologists. The University of Wisconsin-Madison last won the Minnies award in this category in 2017, while the University of Pennsylvania is looking to win its first award ever in this category.
University of Wisconsin-Madison, Madison, WI

The University of Wisconsin-Madison seeks its second Minnies award in this category, with its first coming in 2017. The university offers residency programs in diagnostic and interventional radiology, as well as nuclear medicine.
The diagnostic radiology program accepts eight residents per year for a total of 32 residents who rotate in four-week blocks through various radiology subspecialties over the span of four years. Residents gain experience through a variety of clinical settings including the University of Wisconsin Hospital, American Family Children's Hospital, and facilities operated by the U.S. Department of Veterans Affairs.
The university says it enables growth and capability for residents through structured experiences with progressive independence, including an independent night float experience. The university also takes a subspecialty approach to clinical training and didactics, which allows for residents to focus learning specific areas in radiology before moving on to another organ system.
Program leaders also say all faculty are experienced subspecialists, as well as enthusiastic and engaged to promote deeper learning.
The University of Wisconsin also boasts cutting-edge technology, being the first U.S. institution to treat a patient using the Artis icono biplane angiography system from Siemens Healthineers, used for the first time February 2020.
Along with that, the university highlights its advanced imaging applications. These include a world-renowned virtual colonoscopy program, a tumor ablation program, a robust musculoskeletal ultrasound imaging program, and advances in MRI hardware and software.
University of Pennsylvania, Philadelphia, PA
The University of Pennsylvania (Penn) has achieved numerous accolades in the Minnies awards over the years, with faculty winning radiology researcher awards and its radiological sciences program twice winning the award in that category.
But the title of Best Radiologist Training Program award still eludes the institution. Could this be the year that changes for this Ivy League institution?
The University of Pennsylvania touts its multiple learning tracks and residency programs, with a rich history in the medical field. The university was the first medical school in the U.S. -- the College of Philadelphia, established in 1765 and now the Perelman School of Medicine -- and the first hospital in America (Pennsylvania Hospital).
However, Penn also looks to the future in the form of its residency programs in interventional and diagnostic radiology, with the latter offering clinical and research tracks. Specialty tracks in business and innovation, healthcare leadership, and informatics are also offered, among others.
Additionally, Penn utilizes education innovations in its pedagogy, including personalized teaching sessions, team breakouts, small-group sessions, dedicated minicourses, and flipped classrooms, among other methods. Subspecialty areas, including physics, are also covered.
Residents also gain clinical experience via a diverse case mix from multiple hospitals in and associated with Penn Medicine. This includes reading radiographs, independent call shifts, and working in a night float system. Plus, residents get a slice of life in Philadelphia, the fifth-largest city in the U.S.
Penn Interventional Radiology, meanwhile, contains multiple up-to-date interventional suites. These include one CT-fluoroscopy suite, two C-arm suites, two procedural CT scanners, a preprocedure suite, and a large postprocedure recovery suite. The Perelman Center, meanwhile, has two C-arm suites, a venous ablation suite, and a dedicated interventional radiology clinic with four clinic rooms and provider workroom areas. Ultrasound is also available in all interventional suites and clinics.
Best Radiologic Sciences Program
This year's competition for the Best Radiologic Technologist Training Program is between two juggernauts who have gone head-to-head for the award before, combining for 11 total Minnies in this category. Johns Hopkins University seeks to successfully defend its honor this year, raking in its eighth Minnies award in this category last year. Meanwhile, Thomas Jefferson is looking to dethrone the reigning winners as well as add to its prestige in the annual competition.
Johns Hopkins University, Baltimore, MD

Johns Hopkins University looks to make it two in a row for this Minnies category and its ninth overall in the Best Radiological Sciences Training Program. The university is world-renowned for educating aspiring radiologic technologists while also helping with patient diagnosis and treatment.
The university's radiologic sciences programs train students in radiography, diagnostic sonography, or nuclear medicine over the span of 18 months for all three respective programs. All three programs boast a 100% employment rate within 12 months.
Johns Hopkins also offers advanced programs in CT and MRI that run five and six months, respectively, as well as a mammography training program that lasts for three months.
The university emphasizes hands-on experience for students. To help, the programs boast state-of-the-art medical imaging technology, clinical rotations, and administrative support. These make for an environment for students to undergo theoretical training, whether it be for those just entering the field or those seeking a midcareer change.
Johns Hopkins also offers on-the-job training programs for advanced modalities like MRI, CT, interventional radiology, and mammography. Students also gain firsthand clinical experience at facilities affiliated with the Johns Hopkins system, as well as other clinical facilities throughout the Baltimore/Washington, DC, metropolitan region.
Thomas Jefferson University, Philadelphia PA

Arguably Johns Hopkins' biggest competitor over the years in this category, Thomas Jefferson University (TJU) is seeking its fourth Minnies award in this category, its most recent award coming in 2019.
The university offers bachelor's and master's degrees in radiologic sciences, giving graduates more flexibility when entering the workforce. This includes a single-concentration track for 12 months or a dual-concentration track for 24 months for the bachelor's program. The curriculum integrates didactic, laboratory, and clinical education into its curriculum, and clinical rotations increase over time.
The university's other programs include a CT and PET/CT certificate, two master's degrees in medical imaging and radiation sciences and in medical physics, among others. Concentrations are also offered in radiography, CT, MRI, radiation therapy, medical dosimetry, obstetric/gynecological imaging, and other areas. Management and education tracks are also offered.
TJU highlights its cutting-edge radiology equipment, which gives students hands-on experience. This includes a dosimetry lab with three planning systems, a virtual environment for radiotherapy training, a fetal ultrasound simulator, two mobile x-ray machines (one C-arm, one portable), and a fully equipped radiopharmaceutical laboratory, along with other innovations.
The university also prides itself on the program's 95% to 100% career placement rate since 1995, as well as the 85% pass rate on certification exams for all imaging concentrations.
Most Significant News Event in Radiology
Over two years after the first cases of COVID-19 appeared, the pandemic continued to cast its long shadow on radiology, with supply chain disruptions interfering with availability of iodinated contrast media around the globe. Meanwhile, the first theranostic drug for treating prostate cancer was approved in the U.S. These two developments were picked by the Minnies expert panel as finalists for the Most Significant News Event in Radiology in 2022.
A shortage in the U.S. supply of contrast media
In late April, imaging facilities started scrambling to conserve contrast for CT and x-ray exams after learning GE Healthcare's Omnipaque production facility in Shanghai, China, had shut down due to a local outbreak of COVID-19.
The shortage exposed a weakness in the U.S. supply chain limiting the ability to care for millions of patients and prompted U.S. radiology departments to make dramatic changes in imaging protocols and patient triage.

The ACR offered its recommendations for how to handle the crisis, and the American Journal of Roentgenology published a clinical perspective that stressed the need to assess contrast inventory and cut overall use through tactics such as direct dose reductions, using alternative imaging modalities or contrast agents, or delaying imaging altogether.
The months-long shortage was mostly resolved by the end of June, with GE's Shanghai facility back to normal production, yet supply chain issues lingered.
Ultimately, experts noted the crisis is likely to have long-term effects, in terms of how radiology departments and hospitals around the world stock contrast and where they procure it. It also forced a hard look at how to avoid a similar disruption in the future.
FDA approves Lu-177 PSMA-617 for prostate cancer treatment
March 23, 2022, was a big day in the field of theranostics.
For one, the U.S. Food and Drug Administration (FDA) approved lutetium-177 (Lu-177) prostate-specific membrane antigen radioligand therapy (Pluvicto, Novartis) for the treatment of patients with metastatic prostate cancer.
On the same day, the FDA also approved Novartis' kit (Locametz) for the preparation of the radiotracer gallium-68 (Ga-68) PSMA-11, which is used in PET imaging to identify metastatic prostate cancer tumors.
The approvals mark significant milestones in the emerging field of theranostics -- a term derived from "therapeutics" and "diagnostics" to describe the use of targeted radiopharmaceuticals to both image and treat cancer.
The FDA granted priority review for Lu-177 PSMA-617 in September 2021 based on positive data from the multicenter phase III VISION study. In 800 men with PSMA-positive prostate cancer that had progressed despite standard treatments, 38% showed a reduced risk of death and a 60% reduced risk of progression when treated with Lu-177 PSMA-617.
The new drug is poised to improve outcomes in vast numbers of men, with the American Cancer Society estimating that more than 268,000 new cases of the disease will be diagnosed in 2022.
Biggest Threat to Radiology
Physician burnout

Physician burnout has been named the biggest threat to radiology in each of the past three years by the Minnies expert panel. Will 2022 make it a fourth straight year?
Unfortunately, the signs seem to be pointing in that direction. Physician burnout -- both in radiology and throughout healthcare -- continues to dominate headlines in both the lay press and academic journals. As we've noted in previous Minnies articles, the COVID-19 pandemic has only exacerbated the trend.
Research published in the last year indicates that burnout is a problem not only for physicians but also for radiology staff like radiologic technologists. Many healthcare personnel are trained that the needs of the patient come first, which can make it more difficult to recognize personal feelings of mental and emotional exhaustion.
And burnout isn't just an issue with staff recruitment and retention -- it can also affect patient care itself. A study published in September in BMJ found that patient safety incidents were twice as common among emergency physicians who defined themselves as burned out.
Burnout has also been perniciously resistant to solutions. A study published in Academic Radiology in August 2022 found that solutions implemented at the radiology department level -- such as team-building events, more medical assistants, and an hourly cap on workdays -- didn't make a dent in burnout levels.
Some experts are beginning to believe that efforts to stop burnout need to stop focusing on individual physicians and start addressing changes to the very work culture that's dominant in healthcare.
Corporate takeovers of independent radiology practices

The last time this topic appeared in the finals round of the Minnies was 2019, indicating that traditional economic concerns are beginning to reemerge in radiology as the impact of the COVID-19 pandemic recedes.
Much as was the case three years ago, the Minnies expert panel apparently has concerns about the rise of corporate radiology companies that grow by acquiring traditional radiology practices. The fear is that this trend undermines the independence of radiologists, putting them in the position of essentially being employees of a large corporation.
Much of this trend is being driven by investments made by private equity companies, which are increasingly targeting healthcare as a promising market for investment. In fact, many see radiology in particular as a fragmented market that can easily be consolidated.
Despite some fears related to radiology corporatization trend, some observers see consolidation as promising, giving radiologists access to greater resources -- such as artificial intelligence (AI) deployed at scale -- than many individual groups would be able to achieve on their own.
Hottest Clinical Procedure
Photon-counting CT
Last year's winner of the Minnies award for Hottest Clinical Procedure -- photon-counting CT -- would appear to have the inside track for this year's award as well.
The technology is taking advantage of momentum generated in September 2021, when the FDA cleared the first whole-body photon-counting CT scanner, Naeotom Alpha from Siemens Healthineers. Since then, Siemens has been expanding the installed base of users of the system, and those clinicians have begun producing research papers detailing their experiences with the technology.
The main advantage of photon-counting CT over traditional CT instrumentation is its ability to acquire images at a much higher resolution with a much lower radiation dose. Lower electronic noise, higher iodine signal at higher kV levels, and fewer beam-hardening and metal artifacts are other benefits, according to a recent presentation at the International Society for Computed Tomography (ISCT) meeting.
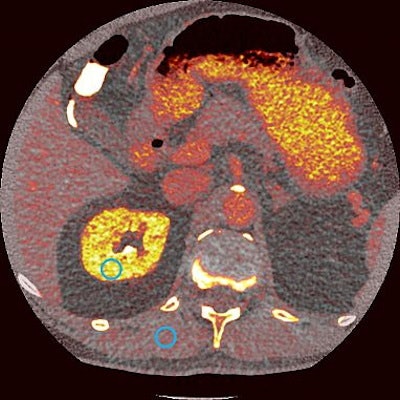 Photon-counting CT offers a wide range of clinical benefits.
Photon-counting CT offers a wide range of clinical benefits.These capabilities produce clinical benefits across a variety of applications, ranging from musculoskeletal to arterial imaging. Recent studies have shown that photon-counting CT can improve imaging in cases of multiple myeloma, visualize cerebrospinal fluid (CSF) venous fistula (CVF) better than traditional CT, and improve diagnosis of interstitial pneumonia.
And Siemens isn't the only company with a photon-counting CT scanner on the market or soon to be available. NeuroLogica announced FDA clearance for its mobile CT system with photon-counting detectors in March 2022, while Canon Medical Systems, GE Healthcare, and Philips have announced their own research projects.
It seems the sky's the limit on the technology the FDA said was the "first major imaging device advancement" in CT in nearly a decade.
Portable MRI
It sounds like a preposterous idea in the era of big-iron MRI scanners at ultrahigh field strengths: build an MRI scanner small enough and light enough that it can be mounted on wheels and transported to the patient's bedside.
But that's exactly what portable MRI is all about. The company that's been most aggressive in popularizing the concept is Hyperfine, which has developed Swoop, a 0.064-tesla scanner that was cleared by the FDA in 2020 and can be plugged into a 110-volt outlet.
 Hyperfine's Swoop portable MRI scanner.
Hyperfine's Swoop portable MRI scanner.Swoop is based on early research conducted at Yale University, and for the past several years, Yale researchers have published a number of papers on the clinical utility of point-of-care MRI. One paper in Resuscitation in July 2022 explored the use of bedside MRI to monitor patients for hypoxic brain injury after cardiac arrest, while an April 2022 paper in Science Advances investigated the technology for bedside evaluation of ischemic stroke.
The scanner is even so portable that it can be sited in a cargo van and transported to patients living in remote areas who may be hours away from the nearest conventional MRI scanner. The system even has potential in developing countries -- it is being tested in the African country of Malawi for detecting cerebral malaria.
Additional exciting applications are possible through the use of AI and machine learning to process low-field images and "upscale" them to appear similar to images acquired with more powerful scanners.
Will portable MRI be able to unseat photon-counting CT as the Hottest Clinical Procedure? Only the Minnies expert panel knows for sure.
Previous page | 1 | 2 | 3 | Next page