VIENNA - When do suspected pulmonary embolism patients actually have pulmonary hypertension (PH)? Although the treatment approach for the conditions is quite different, their presentation can be similar. But a new CT pulmonary angiography (CTPA) tool can accurately predict PH in patients without pulmonary embolism, according to researchers from Israel.
Using a simple prediction model and a tool to automatically measure some vascular parameters, the study team from the Tel Aviv Sourasky Medical Center sorted out the two conditions with nearly 90% sensitivity versus echocardiography.
Sensitivity and specificity "are sufficient to use our model as a screening tool for pulmonary hypertension in patients who undergo CTPA," said lead author Dr. Udi Bendet.
Large volumes of CTPA scans are currently performed to evaluate suspected pulmonary embolism, he said. Pulmonary hypertension may present with similar nonspecific symptoms and be overlooked.
 Dr. Udi Bendet from Tel Aviv Sourasky Medical Center.
Dr. Udi Bendet from Tel Aviv Sourasky Medical Center."Various CT findings are known to suggest the presence of pulmonary hypertension, though there is little research and data concerning the cumulative effect of different CT data relevant to systematic and quantitative diagnosis of pulmonary hypertension," Bendet said. "Our goal was to create a nomogram using cardiovascular data found in CTPA studies for the identification of pulmonary arterial hypertension for patients without acute pulmonary emboli."
Echocardiography was used as a reference test for the presence of pulmonary hypertension, and only patients who underwent both CTPA and echo within 24 hours of each other were included in the study. Patients with inadequate CTPA or echo studies or evidence of acute pulmonary embolism were excluded.
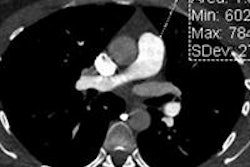
For the CT images, the researchers utilized automated volumetric assessment of the cardiac chambers with investigational software (Comprehensive Cardiac Analysis application, Extended Brilliance Workspace, Philips Healthcare).
The software volumetrically measured right- and left-ventricle diameters and pulmonary artery and ascending aorta diameters, and reflux into the inferior vena cava was graded on a scale of 1 to 6, Bendet said. Pulmonary hypertension was defined as pulmonary artery systolic pressure greater than 33 mm Hg.
"In order to build our model, we used classification trees to divide the predictors into categories based on pulmonary hypertension status," Bendet explained.
Multivariate logistic regression was used to identify predictors of pulmonary hypertension and for building the threshold value that would achieve at least 90% sensitivity so that it could be used as a screening test. The PH prediction model was evaluated with tenfold cross-validation and presented as a nomogram, with the final model used on an additional test group of different patients.
Out of more than 6,000 studies performed, only 370 patients had both tests within 24 hours of each other. After the other exclusions had been completed, the final study group consisted of 182 patients, 54% (n = 98) of whom had pulmonary hypertension based on echocardiography. Patients with PH had a mean age of 75 years, compared with 61 years for those without PH, and there were no significant gender differences.
In the multivariate analysis, the following factors were independently associated with pulmonary hypertension:
- Age ≥ 67 years (odds ratio [OR] 4.46)
- Reflux grade ≥ 3 (OR 2.63)
- Right atrium volume ≥ 106 cm3 (OR 3.59)
- Pulmonary artery diameter ≥ 28 mm (OR 2.52)
- Pulmonary artery/aorta diameter ratio ≥ 0.86 (OR 2.17)
Receiver operator characteristics (ROC) analysis revealed that a threshold of 0.4 provided 90% sensitivity for identifying pulmonary hypertension. Tenfold cross-validation showed 86% sensitivity and 61% specificity, high enough for use as a screening tool, Bendet said.
The group tested the model later on a different cohort of 82 patients using the same criteria, and the results were very similar: Sensitivity was 84.1% and specificity was 60.5%, he said.
"Pulmonary hypertension diagnosis is difficult and is often delayed," Bendet said. "There are reports of some patients being symptomatic for two years before hypertension was diagnosed. We propose an easy-to-use prediction model of pulmonary hypertension for patients who were negative for pulmonary emboli on CTPA."
The main limitation of the study was that it used echocardiography as a reference standard, rather than the gold standard of right-heart catheterization, according to Bendet. Additionally, patients without tricuspid regurgitation were excluded from the study.
"Cardiovascular data derived from CTPA can be utilized to predict PH and to create a nomogram which may facilitate identification of PH after exclusion of acute [pulmonary embolism]," the researchers concluded.