MONTREAL - Radiologists shouldn't be intimidated by artificial intelligence (AI), even though developments in the field are coming at lightning speed, according to Dr. Ronald Summers, PhD, who delivered the opening address at the Canadian Association of Radiologists (CAR) annual meeting on April 26.
Summers, a senior investigator and radiologist at the U.S. National Institutes of Health (NIH), encouraged radiologists to think of AI as a rebranding of computer-aided detection (CAD), and he explained how deep learning will complement the work of radiologists now and in the future.
"It used to be that we had to figure out what we saw in an image and encode that knowledge in terms of mathematics, but we can now take large, annotated sets and feed that into the machine and get out a result," he said. "We can do everything faster."
Hastening progress
Ultimately, the effect of deep learning will be that a wider network of researchers can contribute to knowledge, hastening progress in radiology, according to Summers.
The genesis of deep learning is rooted in the computer vision community, where competitions were launched in an effort to reduce the rate of errors in object recognition. The results of those competitions drove the adoption of deep learning, he said.
One of the earliest examples of machine learning was computer-aided detection of epidural masses, he noted.
"These [epidural] masses were one of the earliest signs of metastases, and they were frequently overlooked because [radiologists] did not always look carefully at the spinal canal," Summers said.
Deep learning is not affecting just radiology, Summers pointed out. Published research involving deep learning has shown that neural networks are as effective as a board-certified ophthalmologist in diagnosing diabetic retinopathy, and they are as accurate as a board-certified dermatologist in diagnosing melanoma (Gushan et al, Journal of the American Medical Association, 2016; Esteva et al, Nature, 2017). And interest in deep learning is growing exponentially, as evidenced by the dramatic growth in the number of articles published in the medical literature on the topic.
Neural networks were employed in the first iteration of deep learning, and they have been supplanted by convolutional neural networks (CNNs), further enhancing object recognition.
"[CNNs] are an improvement on neural networks because they have more layers and permit more levels of abstraction," Summers said.
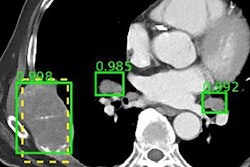
Deep learning is increasing the sensitivity of diagnosis in radiology, such as in the identification of colonic polyps, sclerotic metastases, and lymph nodes (Roth et al, IEEE Transactions on Medical Imaging, 2016).
"With deep learning, we were able to get a 17% improvement [in the detection of colonic polyps measuring 6 mm or larger]," he said.
With an organ like the pancreas, which Summers noted has a wide variety of shapes and thus represents a diagnostic challenge, CNNs have been used to develop a bottom-up approach for organ segmentation using cascaded superpixels and image patch labeling (Roth et al, IEEE Transactions on Image Processing, 2016).
Still another example of the power of computer-aided diagnosis is in identifying a condition such as colitis, where the use of deep learning increased the diagnostic sensitivity to 93.7% (Liu et al, Medical Physics, 2017).
Deep learning is also being harnessed to read radiology reports via natural language processing, but there is far to go before AI is ready to both read reports and images, Summers said. Teaching machines to read radiology reports as well as interpret images would represent a giant leap in radiology, he added.
Should radiologists fear AI?
When asked how radiologists should respond to the growth in AI and whether they should fear AI, Summers said radiologists should choose to embrace deep learning.
"My perspective is that these technologies will enable us to do our jobs better and more accurately," he said. "We are in a phase of a hype cycle where expectations far exceed what the technology can deliver."
For the time being, AI can help with false positives and artifacts, but it is not ready for prime time in the sense that it cannot assist with the prediction of survival or selection of therapy, he explained.
It is not necessary for radiologists, particularly those who are community-based, to retrain and/or become thoroughly familiar with AI. Rather, they can work in collaboration with biomedical engineers or computer scientists to integrate AI in their work.
"Not everyone needs to become an expert," Summers concluded. "I think it is important for radiologists to know if [deep-learning technologies] are working well and if they are validated. Do not be intimidated by this technology just because it is moving at lightning speed."