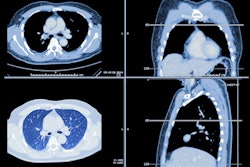
A new study published January 19 in JAMA Internal Medicine links overtreatment of incidental lung nodules found on CT with more radiation, adverse events, and higher health system costs. However, researchers couldn't determine whether or not it also resulted in earlier cancer diagnosis.
The retrospective comparative research study evaluated different management strategies for managing lung nodules incidentally detected on CT in clinical practice at Kaiser Permanente Washington in Seattle and the Marshfield Clinic in Marshfield, WI.
The study feeds into a long-simmering debate about overdiagnosis related to cancer screening, as well as associated harms and costs. Lung nodules are detected incidentally with CT in some 1.6 million people every year in the U.S., but only from 5% to 10% have cancer, the authors noted.
"Clinicians must balance the benefits of prompt lung cancer identification with the risks and costs of diagnostic testing," they wrote.
In the study, the researchers assessed whether management of incidental lung nodules was in line with guidelines at the start of the study period -- 2005 -- and modeled healthcare costs. Not surprisingly, they found a greater number of adverse events, higher radiation doses, and higher costs for management that was more intensive.
The study evaluated patients with incidentally detected lung nodules treated at the two facilities involved in the study between 2005 and 2015, where two-year follow-up data was available. Researchers determined whether practices were in accordance with 2005 Fleischner Society guidelines for managing small pulmonary nodules detected on CT scans.
In the intensely managed group, compared with those managed according to guidelines, researchers expected to see higher costs, radiation exposure, and adverse events, with similar outcomes in terms of the stage of diagnosis. Conversely, in the patients who were managed less intensively, they expected to see lower costs, lower exposure to radiation, and fewer adverse events, but perhaps more people diagnosed with later-stage disease.
Procedure-related adverse events and lung cancer diagnoses were assessed using ICD-9, ICD-10, and Current Procedural Terminology (CPT) codes. Radiation exposure was derived from the number of imaging studies per patient.
Out of the 5,057 with an incidentally detected lung nodule in the study, 38% were managed according to guidelines, 37% were managed less intensively, and 25% were more intensively managed.
Those who had more intensive management had an 8.1% higher rate of procedure-related adverse events compared with those managed according to guidelines. Furthermore, a post-hoc analysis showed that 72% of those who had a procedure-related adverse event did not have a lung cancer diagnosis within a two-year follow-up period.
Other findings are presented in the table below.
| Adjusted 2-year health expenditure comparisons by intensity of nodule evaluation | ||
| Outcome | Less intensive vs. guideline concordant | More intensive vs. guideline concordant |
| Mean difference | Mean difference | |
| Radiation exposure, mSv | -9.5 mSv | +6.8 mSv |
| Health expenditures, 2017 US$ | -$10,916 | +$20,132 |
In fact, costs were estimated to be twice as high for patients whose nodule follow-up was managed more intensively than those managed less intensively -- about $20,000 compared with $11,000 over two years.
"Findings from this study underscore the need to increase the level of evidence that supports current guideline recommendations and decrease unnecessarily intensive diagnostic evaluations of lung nodules," Dr. Farhood Farjah, associate professor of surgery at the University of Washington, and colleagues reported.
The authors believe that the study shows potential harms to patients, which could support quality improvement initiatives.
"For instance, efforts to decrease radiation exposure by approximately 8 milliSieverts may prevent more than 267 radiation-related cancers among the estimated 400,000 people with an incidentally detected lung nodule each year who received more intensive nodule evaluations," they wrote.
However, there were a number of limitations in study design that made it difficult to gauge the impact on the stage of diagnosis for those who did get cancer. The percentage of those who got lung cancer was half the expected rate, and the study was not powered to show if more intensive management resulted in earlier diagnosis and if the reverse was true for less intensive management. The underpowering limited the researchers' ability to "detect small but potentially clinically important differences in stage III or IV lung cancer diagnoses across exposure groups," the authors explained.
Aside from the underpowering of the study, the authors also acknowledged that differences in safety and costs may have been overestimated. Nevertheless, they concluded that the findings have value in showing the use of guidelines in real-world practice and "will have implications for future investigations and quality improvement efforts."
Guidelines can help steer management in the right direction, but adherence varies a lot across practice environments.
"Barriers to adopting guideline-concordant nodule care exist at the patient, clinician, and health system levels, leading to calls for multilevel interventions that can increase guideline-concordant practices," Farjah et al wrote.