Efforts to bring quantitative MRI analysis into clinical practice received a boost with the availability of two new Category III Current Procedural Terminology (CPT) codes for brain MRI.
Effective January 1, 2024, the new codes, 0865T and 0866T, support the use of software to analyze brain MRI exams with comparison to prior studies. AI software would qualify under the Category III CPT codes, which are for new and emerging technology:
The timing of the new codes dovetails with advances in neuroimaging, such as in the assessment of white-matter diseases. As AuntMinnie.com has reported, signs of injury to the brain's white matter called white-matter hyperintensities, as seen on brain scans, may be tied more strongly to vascular risk factors, brain shrinkage, and other markers of neurodegeneration. Radiologists, neurologists, and computer scientists interested in the dynamic patterns of white matter and white-matter lesion distribution in the brain may also want to watch what brain imaging analysis is revealing about white-matter hyperintensities in relation to chronic injuries from sports, blast overpressure effects that lead to "warfighter brain," and a wide variety of other brain imaging applications.
Efforts to bring quantitative MRI analysis into clinical practice received a boost with the availability of two new Category III Current Procedural Terminology (CPT) codes for brain MRI.
Effective January 1, 2024, the new codes, 0865T and 0866T, support the use of software to analyze brain MRI exams with comparison to prior studies. AI software would qualify under the Category III CPT codes, which are for new and emerging technology:
- 0865T -- qMRI analysis of the brain with comparison to prior MR study(ies), including lesion identification, characterization, and quantification, with brain volume(s) quantification and/or severity score, when performed, data preparation and transmission, interpretation, and report, obtained without diagnostic MRI examination of the brain during the same session.
- 0866T -- qMRI analysis of the brain with comparison to prior MR study(ies), including lesion detection, characterization, and quantification, with brain volume(s) quantification and/or severity score, when performed, data preparation and transmission, interpretation, and report, obtained with diagnostic MRI examination of the brain. Health Catalyst explains that 0866T is an add-on code that is used in conjunction with 70551-70553.
The timing of the new codes dovetails with advances in neuroimaging, such as in the assessment of white-matter diseases. As AuntMinnie.com has reported, signs of injury to the brain's white matter called white-matter hyperintensities, as seen on brain scans, may be tied more strongly to vascular risk factors, brain shrinkage, and other markers of neurodegeneration. Radiologists, neurologists, and computer scientists interested in the dynamic patterns of white matter and white-matter lesion distribution in the brain may also want to watch what brain imaging analysis is revealing about white-matter hyperintensities in relation to chronic injuries from sports, blast overpressure effects that lead to "warfighter brain," and a wide variety of other brain imaging applications.
Risk factors
Michael Alosco, PhD, of Boston University and the Chobanian and Avedisian School of Medicine is among those contributing to brain imaging and white matter research.
Using brain MRI scans and lumbar punctures to identify any biomarkers of neurodegenerative disease and white matter changes, Alosco and his collaborators at Boston University have shown associations between repetitive head impacts, white-matter hyperintensities, and brain changes.
What they did: Structural equation modeling tested direct and indirect effects between log-transformed total fluid-attenuated inversion recovery (FLAIR) lesion volumes (TLV) and the revised Framingham stroke risk profile (rFSRP), MRI-derived global metrics of cortical thickness and fractional anisotropy (FA), and CSF levels of beta-amyloid 1-42, p-tau181, soluble triggering receptor expressed on myeloid cells 2 (sTREM2), and neurofilament light.
The researchers made two important points:
- In former football players, a higher level of white-matter hyperintensities was linked to greater vascular risk factors; higher concentrations of p-tau proteins found in Alzheimer's disease, chronic traumatic encephalopathy (CTE), and other neurodegenerative diseases; more brain shrinkage; and a decrease in the health of the white matter pathways in the brain.
- The relationship between white-matter hyperintensities and stroke risk was 11 times stronger in former football players than in those who did not play football, 2.5 times stronger for the concentration of p-tau proteins, and four times stronger for white matter integrity.
"In addition to vascular health, p-tau 181 and diffusion tensor imaging indices of white matter integrity showed stronger associations with WMH in the former football players. FLAIR WMH may have specific risk factors and pathologic underpinnings in [repetitive head impact] RHI-exposed individuals," Alosco's team concluded in their article published in December 2023 in Neurology. The work builds on previous research. In 2018, Alosco received nearly $800,000 from the National Institutes of Health's National Institute of Neurological Disorders and Stroke for the research.
Gray matter-white matter integrity
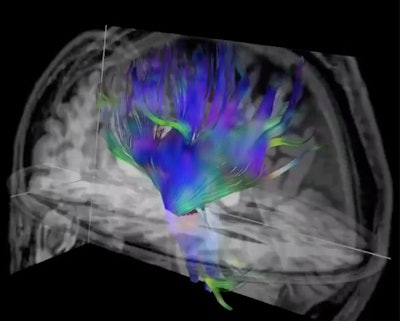 Researchers used diffusion-tensor imaging, an MRI technique, to study the impact of soccer heading on the brain. This method tracks the microscopic movement of water molecules through brain tissue to characterize the brain's microstructure. Image and caption courtesy of the RSNA.
Researchers used diffusion-tensor imaging, an MRI technique, to study the impact of soccer heading on the brain. This method tracks the microscopic movement of water molecules through brain tissue to characterize the brain's microstructure. Image and caption courtesy of the RSNA.
At New York University (NYU) Presbyterian, Molly Charney, MD, and colleagues are using diffusion tensor imaging (DTI) MRI to study brain injuries from sports, specifically related to soccer heading. With DTI-MRI, researchers can track microscopic movement of water molecules through brain tissue. In this way, they can look for associations between characteristics of changes in the brain microstructure and cognitive performance.
What they found: Imaging analysis indicated declines in the brain microstructure and function related to a high amount of soccer heading. Normally sharp gray matter-white matter interface was blunted.
“We used DTI to assess the sharpness of the transition from gray matter to white matter," explained senior author Michael Lipton, MD, PhD, in a statement from the RSNA. Lipton is a professor of radiology at Columbia University’s Vagelos College of Physicians and Surgeons and an affiliate professor of biomedical engineering at Columbia University. "In various brain disorders, what is typically a sharp distinction between these two brain tissues becomes a more gradual, or fuzzier transition."
The study focused on 148 soccer players with an average age of 26.7 years. Questionnaire data categorized their repeated head impacts as low (0-556 total headers), moderate (564-1,512 total headers), or high (1,538-23,462 total headers) over a two-year period. High levels of heading over the study were associated with brain microstructure changes similar to mild traumatic brain injuries.
“There is enormous worldwide concern for brain injury in general and in the potential for soccer heading to cause long-term adverse brain effects in particular,” Lipton said. The results of the study suggested that greater heading exposure over two years is associated with adverse effects on white-matter microstructure.
Role for PET
At the University of Virginia (UVA), researchers are using PET to investigate "warfighter brain," a military brain condition caused by stressful injury to the brain from outward force, oftentimes due to a blow to the head or a violent movement of the head. The U.S. Department of Defense's Warfighter Brain Health Initiative has launched 26 health and performance studies focused on blast overpressure.
One study could help determine how long military members should stay in the blast environment and prevent traumatic brain injury. Lead author James Stone, MD, and colleagues at UVA Health looked at the common thread of neuroinflammation that appears to follow blast overpressure and repeated exposure to low-intensity blasts.
A widely used class of radiopharmaceuticals in the study of the neuroinflammatory response targets the translocator protein (TSPO), according to the researchers. Within the brain, TSPO is found within microglia and demonstrates significantly increased expression within activated microglia. As such, radiopharmaceuticals consisting of a TSPO ligand coupled to a PET radioisotope serve as effective imaging agents for neuroinflammation.
Why it matters: The researchers said the emerging evidence suggests neuroinflammation may be a key feature of the brain response to blast exposure over a career in operational personnel. The common thread of neuroinflammation observed in blast-exposed populations requires further study. The researchers also noted this is the first work to explore neuroimaging-derived critical generalized blast exposure value thresholds, and they noted a relationship between these thresholds and white-matter integrity.
"Neuroinflammation levels, on their own, do not differ substantially between more highly and less highly exposed participants after controlling for potential confounds," the researchers wrote. "However, within the exposed cohort, PET neuroinflammation measurements increase significantly with higher exposure levels. Additionally, MRI measurements demonstrate that increased blast exposure relates to reductions in volume and thickness of brain structures," the authors continued. "These findings, together, establish that GBEV may provide an index into underlying effects of blast overpressure."
The study was published January 12 in the Journal of Neurotrauma.
Other applications
Researchers are also demonstrating the value of quantitative MRI in a wide variety of other brain imaging applications, such as using AI with DTI-MRI to show differences in the brains of children with and without ADHD, to diagnose autism, in revealing brain changes in people with long COVID, assisting in diagnosis of Alzheimer's disease during PET/MRI scans, screening of patients with suspected cerebrospinal fluid disorders, illuminating gray-matter changes in diabetic patients, identifying biomarkers that predict multiple sclerosis progression, and in patients with post-traumatic stress disorder (PTSD).
