AI reduces breast radiologist workload while also improving screening performance and decreases the number of false-positive findings, according to a study published June 4 in Radiology.
A team led by Andreas Lauritzen, PhD, from the University of Copenhagen in Denmark found that the commercially available AI system used in a population-based mammography study led to a 20% decrease in the recall rate and a 33% decrease in reading workload.
“I think [AI] will add a lot of value to the radiologists themselves, where they have the tools and they can see markings from the AI,” Lauritzen told AuntMinnie.com. "They can prioritize their time and resources to the cases that actually matter."
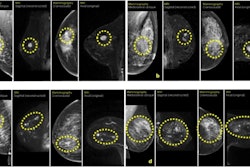
Retrospective studies have suggested that using AI can lessen the burden radiologists face when interpreting mammograms. Lauritzen and colleagues added that AI systems could serve as supportive tools for stratifying screenings based on breast cancer probability -- a possibility that has motivated exploration of their use in population-based breast cancer screening.
The researchers hypothesized that letting radiologists read mammograms with AI-assisted decision support and AI-provided lesion markings could increase screening sensitivity. They performed a study for which they compared workload and screening performance for two patient cohorts who underwent screening before and after the implementation of an AI system (Transpara v.1.7.1, ScreenPoint Medical).
The work included data collected between 2020 and 2023 from 60,751 women who underwent biennial screening before AI system implementation and 58,246 women who were screened after implementation. The women had a median screening interval before AI of 845 days and with AI of 993 days (p < 0.001).
Before AI system implementation (2020 to 2021), all screenings involved double reading. For screenings conducted after AI system implementation (2021 to 2022), “likely normal” screenings were single-read by one of 19 senior full-time breast radiologists.
The remaining screenings were read by two radiologists with AI-assisted decision support. Biopsy and surgical outcomes were retrieved between 2020 and 2023, ensuring at least 180 days of follow-up.
The team reported that the AI system implementation led to decreases in the recall rate, false-positive rate, and radiologist workload. It also reported increased cancer detection rate, positive predictive value, and the rate of small cancers.
| Effect of AI implementation on breast cancer screening measures | |||
|---|---|---|---|
| Measure |
Before AI |
After AI |
p-value |
| Recall rate |
3.1% |
2.5% |
< 0.001 |
| Cancer detection rate |
0.7% |
0.82% |
0.01 |
| False-positive rate |
2.4% |
1.6% |
0.001 |
| Positive predictive value |
22.6% |
33.6% |
< 0.001 |
| Rate of small cancers (≤ 1 cm) |
36.6% |
44.9% |
0.02 |
| Rate of node-negative cancers |
76.7% |
77.8% |
0.73 |
| Rate of invasive cancers |
84.9% |
79.6% |
0.04 |
AI implementation also led to the reading workload being reduced by 33.5% (38,977 of 116,492 reads).
The study authors wrote that future work should evaluate screening sensitivity, specificity, interval cancer rate, and the impact of higher ductal carcinoma in situ (DCIS) detection.
“Around November 2024, we will have full two-year follow-up data for the cohort of women screened with AI,” they wrote. “Further, in future work, we aim to quantify the effects of AI stratification, AI decision support, and radiologist access to prior screenings separately.”
Lauritzen said that the team doesn’t plan to implement other AI systems into their research.
In an accompanying editorial, Amie Lee, MD, from the University of California, San Francisco, and Sarah Friedewald, MD, from Northwestern University in Chicago wrote that the Lauritzen team’s study adds evidence to AI’s capabilities in breast imaging. However, they cautioned that implementing different versions of AI tools could lead to variable performance and that increased cancer detection alone is “not an acceptable proxy for the outcome of most interest, decreased mortality.”
“The types of cancers detected [tumor biology, size, grade, and node positivity] must be more rigorously studied,” Lee and Friedewald wrote. “Further studies are necessary to demonstrate the benefits of AI in other screening environments.”
The full study can be found here.