High-volume teleradiology requires some adjustments in a department's workflow; in particular, radiologists have to keep a close eye on factors such as image quality and workstation interface parameters. But the benefits are worth the effort, according to researchers from the University of Arizona in Tucson, AZ.
"Overall, teleradiology is a positive experience," said research professor Elizabeth Krupinski, Ph.D. "Most staff participate and are generally satisfied."
Krupinski presented an update from a 1998 study examining radiologist satisfaction with teleradiology at the 2003 Symposium for Computer Applications in Radiology in Boston. After a pilot study in 1996, the university formally launched its teleradiology services in 1997, and now provides services to 22 sites in Arizona and New Mexico.
The institution's teleradiology case volume has climbed significantly in the past few years as new sites came online and the radiologists begin reading all of the cases for some locations. In 2002 they read nearly 60,000 cases, more than seven times the caseload in 1998. And the university is well on track to exceed that figure in 2003, Krupinski said.
Through the program, University of Arizona radiologists are available to provide both second opinion and primary diagnosis for all modalities on a 24/7 basis. Part of the Arizona Telemedicine Network, the teleradiology service takes advantage of an ATM T1/T3-based network.
The institution employs RadWorks software (GE Medical Systems, Waukesha, WI), as well as both monochrome and color cathode-ray tubes (CRTs) and liquid crystal displays (LCDs). Radiologists provide reports using IBM’s MedSpeak speech recognition software and a Web-based reporting application developed in-house by the university.
Most of the teleradiology involves plain-film or computed radiography cases, followed by CT, ultrasound, mammography, MR, and nuclear medicine studies.
In light of such dramatic gains in image volume, the group decided to reevaluate radiologists' satisfaction with the teleradiology service. This was accomplished by updating the 1998 survey and adding two new questions. Thirteen queries were Likert-scale questions, while two were open-ended.
The survey was sent to all radiology personnel at the university, with 31 (94%) responding. Of the 31, 21 perform teleradiology reading services, including 65% of attending physicians and 60% of residents.
In the 1998 study, 63% of survey respondents had rated image quality as excellent or good, with 90% judging system friendliness to be excellent or good. Readers rated their diagnostic confidence as approximately the same as film in 32% of cases, while 68% had lower confidence than with film.
"That was when we were just starting out, and that might be a little bit due to inexperience," Krupinski said. "But the image quality wasn’t really there as well."
In cases that produced low confidence by the radiologists, 71% cited poor image quality, 14.5% noted no clinical history, and 14.5% said there weren't enough images. Twenty-six percent of respondents reported having a case they couldn’t read due to poor image quality. This situation, however, occurred only in about 5% of cases, she said.
Update 2002
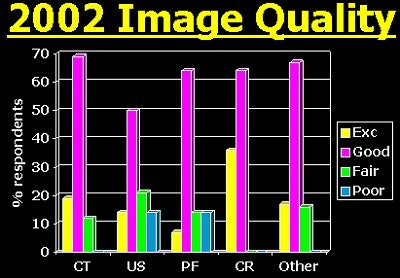
In 2002, image quality was rated highest in the digital images (computed radiography, full-field digital mammography, CT, MR), Krupinski said. Digitized studies (plain-film and ultrasound exams), were a problem area, however.
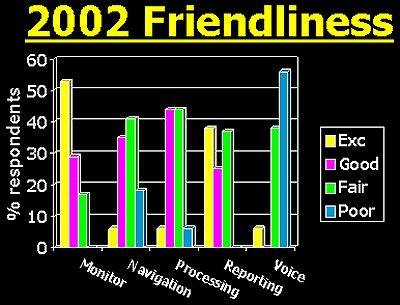
As for system friendliness, the speech recognition component fared poorly, with most radiologists rating it fair to poor, Krupinski said. There are several reasons why radiologists don’t like the system, including an unwillingness to take the time to practice, Krupinski said.
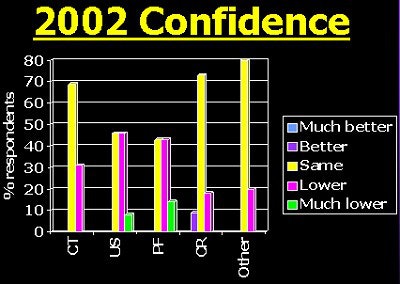
Diagnostic confidence was very similar to the 1998 survey.
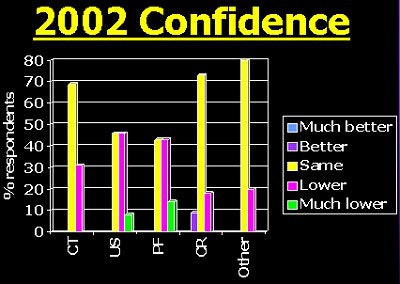
The researchers found only moderate correlation between image quality and confidence in the 2002 data. Attendings and residents had approximately the same correlation.
Sixty-two percent said they had cases they could not read. Of these, 94% reported having an unreadable case in 1%-10% of cases, with 6% finding an unreadable case in 21%-30% of cases, she said.
Ninety-two percent of both attending physicians and residents cited image quality as the reason for unreadable cases, with 85% of attendings reporting not enough images and 46% of attendings pointing to a lack of clinical history.
In other 2002 results, the researchers discovered that 33% were given background information on the rural sites from which they were receiving images. Seventy-one percent of respondents (including 93% of attendings and 17% of residents) were interested in understanding how their work contributes, Krupinski said.
Overall, teleradiology is a good source of revenue and teaching material, she concluded. Not only does it provide a good learning experience, it enhances the diversity of cases with more variation in disease, she said.
Most staff use and are generally satisfied with the system. However, some work is needed on the system, and some modalities are better than others, Krupinski said.
By Erik L. RidleyAuntMinnie.com staff writer
September 19, 2003
Related Reading
Teleradiology benefits Balkans, June 11, 2003
Working through the politics of PACS, June 6, 2003
Separating HIPAA facts from fiction, May 12, 2003
Legal ground rules guide international teleradiology practice, February 20, 2003
Copyright © 2003 AuntMinnie.com




















