NEW ORLEANS - The Alaska Federal Health Care Access Network (AFHCAN) has successfully employed telehealth technology that has boosted efficiency, cut costs, and improved patient care, according to AFHCAN director Stewart Ferguson, Ph.D.
The largest U.S. state in land mass, Alaska faces a number of healthcare challenges, including weather issues, prevalence of remote clinics, and a shortage of healthcare professionals. Approximately two-thirds of the population are in underserved areas, and 49% of physicians in Alaska are primary care physicians (compared with the U.S. average of 28%), said Ferguson, who spoke during a session Monday at the Healthcare Information and Management Systems Society (HIMSS) conference.
"About two-thirds of our physicians are located in Anchorage," he said. "What that means is if you want any kind of specialty care, you pretty much have to travel to Anchorage."
Launched in 1998 to develop and employ telehealth technology, AFHCAN is a large-scale, multiagency, and multiprovider effort. It encompasses 248 sites, over 500,000 square miles, 43 autonomous organizations, three federal agencies, and providers such as community health aide/practitioners (CHA/P) and nurses.
When asked what their key organizational goals were for telehealth applications, participating organizations listed quality of care as their top priority, followed by access to care and patient satisfaction, Ferguson said.
Of AFHCAN's 248 sites, 158 (67%) are staffed by CHA/Ps. Only 11% of these sites are accessible by road, and 70% require small plane or helicopter access.
Workflow challenges
The project focused on integrating with the way providers work, and formalizing relationships and mutual responsibilities, according to Ferguson. It supports existing referral patterns, with software that enables and facilitates healthcare delivery without generating new business rules, he said.
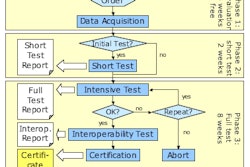
"We've developed a multiserver system, including an enterprise system where everybody got their own server," he said. "They can set up 'trust' relationships with any other server on the network. When they do that, they can send cases to those organizations."
The project supports existing network designs, conforming with all firewalls and routers in the 43 participating organizations, Ferguson said.
AFHCAN wanted to design the user interface for the user, focusing on simplicity and minimizing the need for keyboard skills. The final product features a touch screen and color coding, and users can create a case in five to 10 minutes, Ferguson said.
The cart serves as a primary care tool, and can help in applications such as ear disease, heart disease, respiratory illness, trauma, and dental applications, he said.
The telehealth project has led to improved efficiency, reduced cost of care, increased patient throughput, benefits for presurgical planning and postsurgical follow-up, and better triage decisions, he said.
"Most importantly, you can empower people who are not high-level, highly paid specialists to provide care and to develop alternate service delivery models," he said.
Telehealth has also led to reductions in the cost of healthcare, Ferguson said. A survey of users found that the telemedicine case/image prevented patient travel in 49% of 8,567 cases. Recently, that number has climbed as more tertiary care centers have come online, up to an average of 68% in the last year, Ferguson said.
From that data, AFHCAN estimates that annual savings from the telehealth system most likely ranges from $3 million to $9 million, a figure that would be higher if lodging and per diem were included.
Reimbursement is also not an issue for AFHCAN. From a review of 1,076 claims, AFHCAN found that 977 (91%) of the claims that were submitted were paid. Of the 99 claims that weren't, 61 of the patients were ineligible or the deductible hadn't been met, Ferguson said.
The data also revealed a surgical preplanning benefit from the telehealth system. A review of 56 telehealth cases that led to direct surgical referrals found 92.9% accuracy in predicting the procedure and a 31-minute average difference in predicted versus actual operating time. In comparison, a matched selection of 56 nontelehealth surgical referrals had 87.5% accuracy in predicting the procedure, and a 36-minute average difference in predicted versus actual operative time, Ferguson said.
After surgery, telehealth provides the ability to monitor and follow-up these patients, which has traditionally been difficult for patients from remote settings, he said.
When asked in a survey if telemedicine would improve the quality of care for the patient after a telemedicine case was generated, users said that it would in 86% of the cases, Ferguson said. When asked if telemedicine made their job fun, 77% of the respondents also said yes.
Sixty-four percent of cases played a role in educating the patient, and 78% were rated as improving patient satisfaction, he said.
By Erik L. Ridley
AuntMinnie.com staff writer
February 27, 2007
Related Reading
U.S. takes steps to ramp up HIT efforts, February 23, 2007
CCHIT certifies 18 EHR products, January 30, 2007
CCHIT releases interoperability test scripts, data files, January 5, 2007
CCHIT expands EHR certification to specialties, December 15, 2006
Bill passed to require EHR capabilities for federal employees, September 14, 2006
Copyright © 2007 AuntMinnie.com